You’ve probably had that uncomfortable moment: a sudden itch, a rash, or even persistent dryness that seems to come out of nowhere. These might be more than just fleeting skin troubles; they could be signs of Atopic Dermatitis (AD). This condition, more commonly known as eczema, affects many and might affect you or someone you know.
Behind every itch or rash lies a story waiting to be told. Are you ready to listen to what yours might be saying? Every line ahead holds a clue.
What is Atopic Dermatitis?
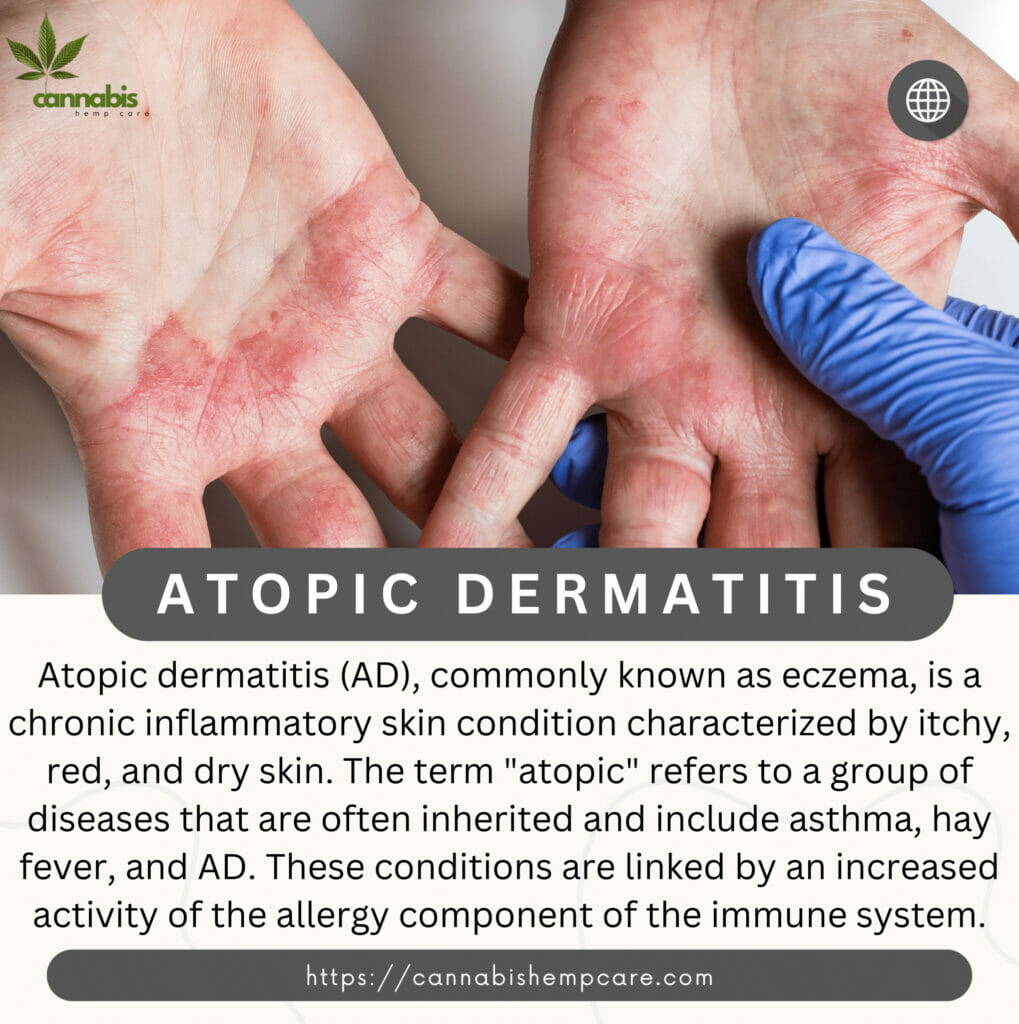
Atopic dermatitis (AD), commonly known as eczema, is a chronic inflammatory skin condition characterized by itchy, red, and dry skin. The term “atopic” refers to a group of diseases that are often inherited and include asthma, hay fever, and AD. These conditions are linked to an increased activity of the allergy component of the immune system.
Atopic Dermatitis vs Eczema
See how these skin conditions differ in the table below.
| Categories | Eczema | Atopic Dermatitis (AD) |
|---|---|---|
| Definition | A general term for chronic skin conditions marked by itchiness and inflammation. | The most common form of eczema. Often starts in childhood and can be linked to other allergic conditions like hay fever and asthma. |
| Differences | Both are characterized by itchy, inflamed skin. | While both are characterized by itchy, inflamed skin, AD is typically more severe. It might have specific triggers not present in other eczema types. |
| Treatment | Both require symptom management. | AD might need a more comprehensive approach due to its severity and potential link to allergens. |
Not all eczema is AD. Knowing the distinction helps in targeted treatment and better management.
Characteristics and Symptoms
Atopic Dermatitis (AD) showcases a range of symptoms that may fluctuate in intensity over time. Here are the primary characteristics and symptoms associated with AD:
- Itchy Skin:
- Often the initial and most noticeable symptom.
- Severity can range from mild to intense and may persist over time.
- Often the initial and most noticeable symptom.
- Redness and Swelling:
- Skin in affected areas may turn red and swell.
- Small, fluid-filled blisters might form.
- Skin in affected areas may turn red and swell.
- Dry Skin:
- Characterized by a dry, possibly scaly texture.
- Tendency to crack or flake.
- Characterized by a dry, possibly scaly texture.
- Inflammation:
- A distinguishing feature of AD, exacerbating itchiness and other symptoms.
- A distinguishing feature of AD, exacerbating itchiness and other symptoms.
- Skin Thickening (Lichenification):
- Repeated scratching and rubbing can lead to thickening of the skin.
- Can create a leathery texture, further perpetuating the cycle of itchiness.
- Repeated scratching and rubbing can lead to thickening of the skin.
Understanding these symptoms can provide insight into the management of AD and improve the quality of life for individuals affected by this condition.

Causes
Atopic Dermatitis (AD) arises from various factors. Here are the primary causes:
- Genetics:
- Higher risk if family members have eczema, asthma, or hay fever.
- Higher risk if family members have eczema, asthma, or hay fever.
- Environment:
- Dry climates, high pollution, and cold temperatures can worsen AD.
- Dry climates, high pollution, and cold temperatures can worsen AD.
- Skin Barrier:
- Defective barriers make skin more prone to irritants.
- Defective barriers make skin more prone to irritants.
- Immune System:
- Abnormal responses can lead to AD symptoms.
- Abnormal responses can lead to AD symptoms.
- Allergens:
- Triggers include pollen, dust mites, mold, pet dander, and certain foods.
- Triggers include pollen, dust mites, mold, pet dander, and certain foods.
Understanding these causes aids in better managing and treating AD, allowing individuals to minimize exposure to triggering factors potentially.
Food Triggers
Certain foods can exacerbate Atopic Dermatitis (AD) symptoms in some individuals. Here’s a list of common food triggers:
- Dairy Products: Milk, cheese, and other dairy products can be problematic for some people with AD.
- Eggs: Mainly the proteins in egg whites can be a trigger.
- Nuts and Seeds: Peanuts, walnuts, and sesame seeds are among the common culprits.
- Soy: Found in various products, soy can be a potential allergen for some.
- Wheat: Gluten, a protein in wheat, might exacerbate AD in some individuals.
- Fish: Certain types of fish, especially shellfish, can trigger reactions.
- Citrus Fruits: Oranges, lemons, and other citrus fruits can irritate some people’s skin.
It’s important to remember that not everyone with AD will be affected by these foods. If you suspect a food trigger, consult a healthcare professional before making dietary changes.

Stage of Atopic Dermatitis
Atopic Dermatitis (AD) progresses through various stages, presenting different symptoms and challenges. Understanding these stages can aid in managing the condition effectively.
- Infantile Stage (0-2 years):
- Often appears as red, itchy, and scaly patches, mainly on the cheeks, scalp, or limbs.
- Itching can lead to skin infections if the skin is broken from scratching.
- Often appears as red, itchy, and scaly patches, mainly on the cheeks, scalp, or limbs.
- Childhood Stage (2-12 years):
- AD may spread to the neck, hands, feet, or eyelids.
- The skin may become lichenified (thickened) from constant itching and rubbing.
- AD may spread to the neck, hands, feet, or eyelids.
- Adolescent/Adult Stage (12 years and older):
- AD might persist, improve, or clear entirely.
- Common areas affected include the face, neck, hands, and the crooks of elbows and knees.
- AD might persist, improve, or clear entirely.
Understanding and managing Atopic Dermatitis (AD) is vital for maintaining skin health and overall well-being. By recognizing its stages and triggers, individuals can better navigate this condition. Always consult with a dermatologist for tailored advice and treatment options.
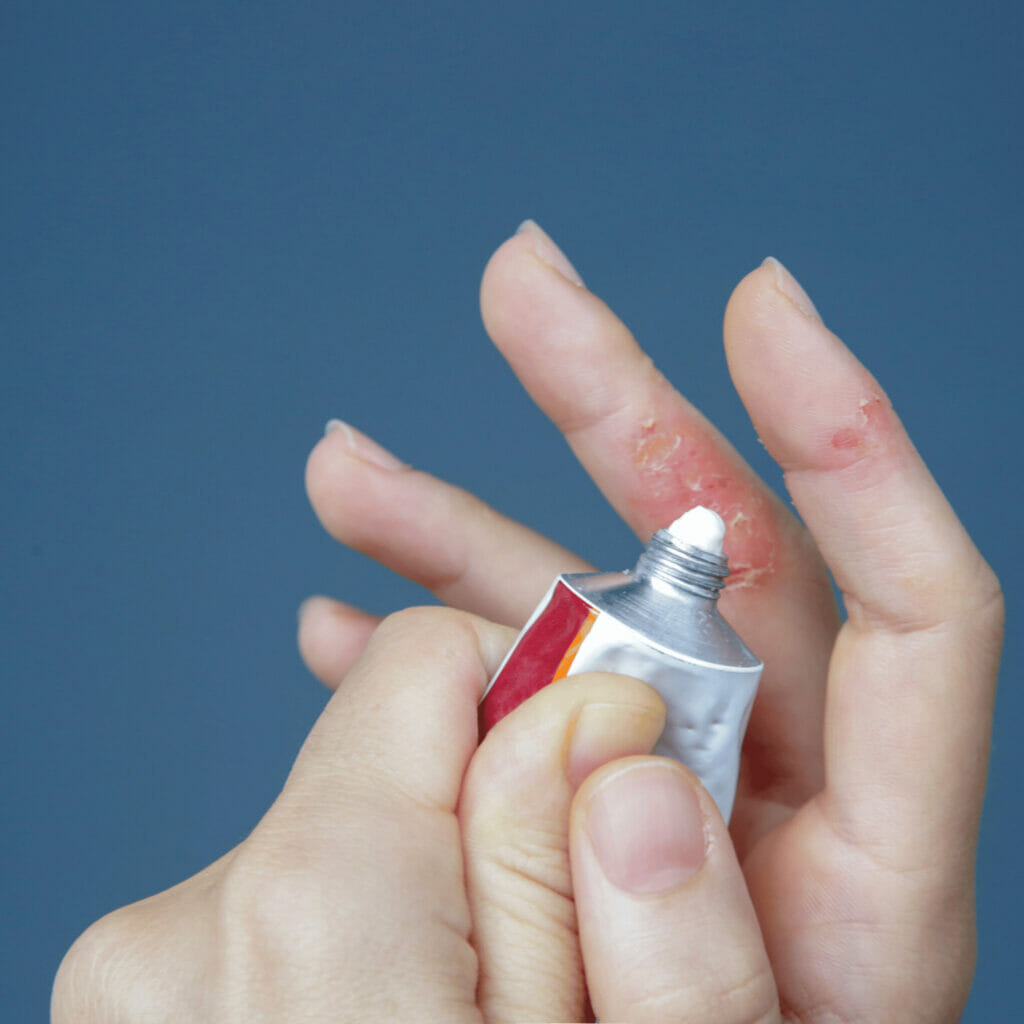
Treatment
Effective AD treatment involves preventive steps and medication. Key treatments include:
- Moisturizing
- Regularly applying moisturizers can prevent dryness and reduce the severity of outbreaks.
- Regularly applying moisturizers can prevent dryness and reduce the severity of outbreaks.
- Topical corticosteroids
- These are used to reduce inflammation and itching.
- These are used to reduce inflammation and itching.
- Topical calcineurin inhibitors
- Such as tacrolimus and pimecrolimus can be used as alternatives or in combination with corticosteroids.
- Such as tacrolimus and pimecrolimus can be used as alternatives or in combination with corticosteroids.
- Topical PDE4 inhibitors
- Crisaborole is an example, which reduces inflammation.
- Crisaborole is an example, which reduces inflammation.
- Systemic treatments
- In severe cases, oral corticosteroids or other immunosuppressant drugs like cyclosporine might be prescribed.
- In severe cases, oral corticosteroids or other immunosuppressant drugs like cyclosporine might be prescribed.
- Dupilumab
- An injectable biologic therapy that targets specific inflammatory pathways.
- An injectable biologic therapy that targets specific inflammatory pathways.
- Phototherapy
- Exposing the skin to controlled amounts of natural or artificial light.
- Exposing the skin to controlled amounts of natural or artificial light.
Complications
AD isn’t just about itchy skin. It can lead to further issues, including:
- Asthma or Hay Fever:
- Increased risk with AD.
- Increased risk with AD.
- Chronic Itchy, Scaly Skin (Neurodermatitis):
- May develop from AD.
- May develop from AD.
- Skin Infections:
- Constant scratching can cause open sores, leading to infections.
- Constant scratching can cause open sores, leading to infections.
- Eye Complications:
- Includes blepharitis, conjunctivitis, and keratoconus.
- Includes blepharitis, conjunctivitis, and keratoconus.
Prevention
Atopic Dermatitis (AD) can be a persistent challenge, but understanding its prevention can make a significant difference. Simple daily practices can mitigate its onset or severity.
- Moisturize: Daily routine.
- Bathing: Short, lukewarm sessions.
- Cleansers: Opt for gentle, unscented types.
- Clothing: Choose soft, breathable fabrics.
- Avoidance: Steer clear of known triggers like specific foods and allergens.
Managing AD is more feasible when armed with knowledge of prevention. Adopting these measures can pave the way for healthier skin and reduced flare-ups.
When to see a doctor?
Atopic Dermatitis (AD) can be a relentless condition, making the decision of when to seek medical attention crucial. Recognizing persistent or worsening symptoms is the first step toward getting appropriate care.
- Persistent Symptoms
- If itching and redness don’t improve or persist despite home care.
- If itching and redness don’t improve or persist despite home care.
- Sleep Disruption
- When symptoms interfere with sleep regularly.
- When symptoms interfere with sleep regularly.
- Skin Infections
- Signs of infection include increased redness, warmth, pus, or yellowish crust.
- Signs of infection include increased redness, warmth, pus, or yellowish crust.
- Unidentified Triggers
- When you’re unable to pinpoint what’s causing flare-ups.
- When you’re unable to pinpoint what’s causing flare-ups.
- Treatment Ineffectiveness
- Over-the-counter treatments don’t provide relief or symptoms worsen.
- Over-the-counter treatments don’t provide relief or symptoms worsen.
- Quality of Life Impact
- When AD starts affecting daily activities or emotional well-being.
- When AD starts affecting daily activities or emotional well-being.
Knowing when to seek medical help is key to better control and management of AD.

Final Thoughts
Living with atopic dermatitis can be challenging due to the persistent itch and cosmetic concerns. Support groups and counseling can help patients and families cope with the emotional aspects of the condition. It’s also essential to consult with a dermatologist for a proper diagnosis and treatment plan.