Ever found yourself resisting the urge to scratch that persistent itch or gazing in the mirror at a patch of skin that just won’t clear up? Eczema, a common skin ailment, remains enigmatic to many.
This guide delves deep into its causes, highlights potential triggers, and offers insights on effective management strategies. If you’ve ever wondered about the link between your diet and those pesky flare-ups or felt overwhelmed by the maze of treatments available, you’re in the right place.
Equip yourself with knowledge, and take control of your skin’s health. Ready to get started?
What is eczema?
Eczema, also known as atopic dermatitis, is a chronic skin condition characterized by inflamed, itchy, and dry patches of skin1. The condition often presents in cycles, with periods of flare-ups followed by remission. While the exact cause remains unclear, a combination of genetic and environmental factors plays a role in its development.
Eczema is not a contagious condition2. Although there is no definitive cure, various treatments aim to alleviate symptoms and prevent flare-ups. Factors such as irritants, allergens, and stress can exacerbate the condition. Proper skin care and medical interventions can help manage its effects.
7 Types of Eczema
Eczema is more than just a singular skin condition; it’s a group of skin disorders that cause inflammation, itchiness, and redness. Below are the various types of eczema explained.
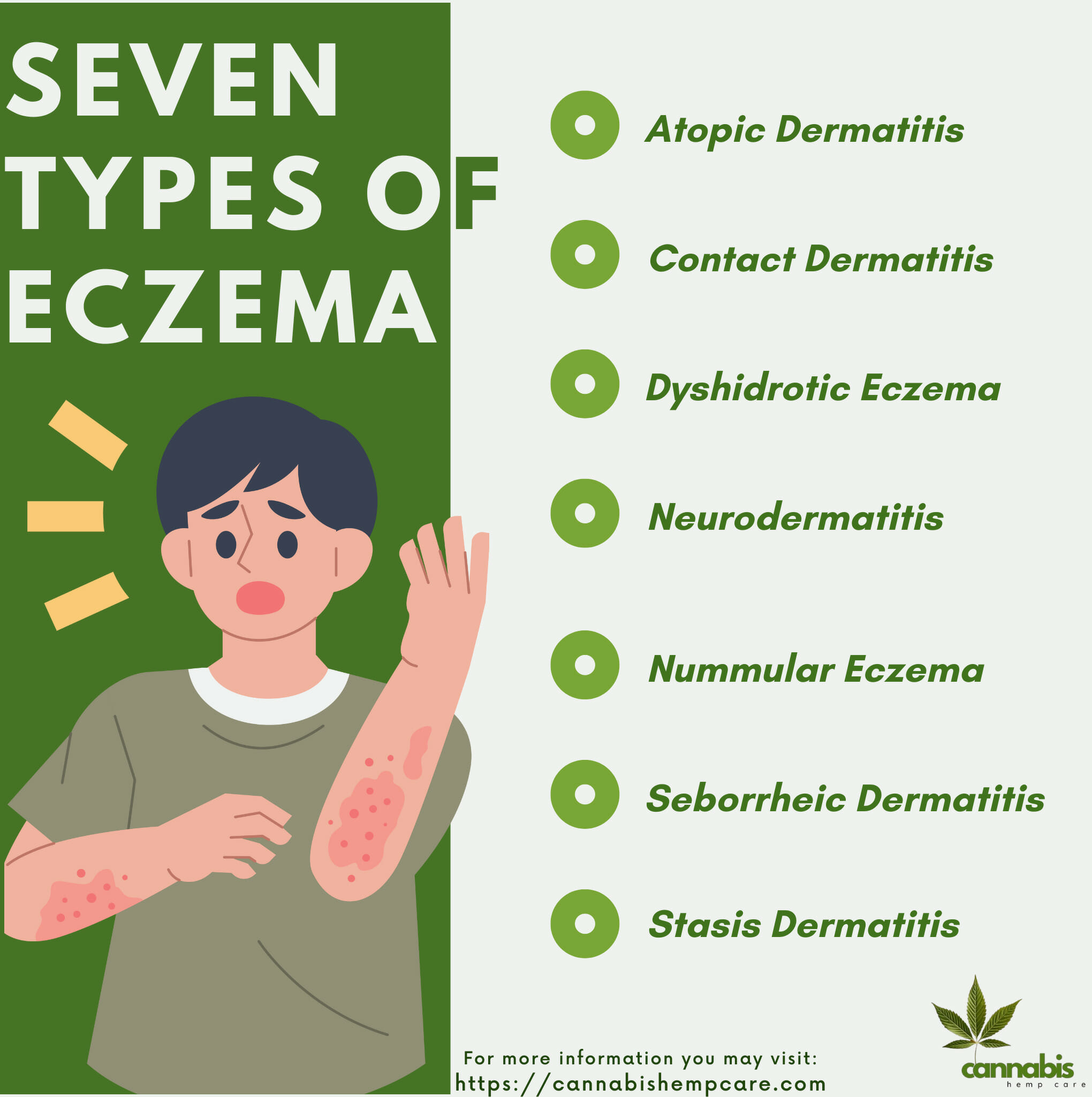
1. Atopic Dermatitis
The most common form of eczema is often linked with other allergic conditions such as asthma and hay fever. It presents as dry, itchy, and inflamed skin.
2. Contact Dermatitis
This type arises from direct contact with irritants or allergens, like chemicals or nickel, causing skin irritation or allergic reactions respectively.
3. Dyshidrotic Eczema
Characterized by small, itchy blisters on the edges of the fingers, toes, palms, and soles of the feet, which can be painful.
4. Neurodermatitis
Triggered by intense itching, affecting 12% of the population. The skin in affected areas often shows visible lines, scales, and discoloration from excessive itching. Common sites include the feet, ankles, hands, wrists, elbows, shoulders, neck, and scalp.
5. Nummular Eczema
Identifiable by round, coin-shaped spots on the skin, often appearing after a skin injury such as a burn or abrasion.
6. Seborrheic Dermatitis
Mainly affects the scalp leading to dandruff, but can also cause red, scaly patches on the face, especially around the nose and eyebrows.
7. Stasis Dermatitis
Associated with blood flow issues in the veins of the lower legs, leading to fluid buildup, itching, and reddish-brown discoloration of the skin.
Each type of eczema has unique symptoms and may require different types of treatment. It’s crucial to consult with a dermatologist for an accurate diagnosis and appropriate management plan.
Symptoms
Eczema is a skin condition known for its itching and inflammation. While it can affect individuals of all ages, the symptoms can manifest differently across age groups3. Here’s a breakdown:
| Age Group | Symptoms | Description |
|---|---|---|
| Infants | Rash | Commonly appears on the face and scalp, sometimes extending to other areas of the body. |
| Itching | Extreme itchiness which may interfere with sleeping. | |
| Bumps | Bumps that can ooze fluid and crust over when scratched. | |
| Children | Rashes | Increased risk of skin infections and eruptions can be more scaly and cover larger areas than in children. |
| Bumpy Skin | Skin can become bumpy and can lighten or darken in color. | |
| Itching | Persistent itching which can be severe during flare-ups. | |
| Adults | Dry Skin | Extremely dry skin over large areas of the body. |
| Itching | Increased risk of skin infections and eruptions can be more scaly and cover larger areas than in children. | |
| Infections | Increased risk of skin infections, and eruptions can be more scaly and cover larger areas than in children. |
It’s crucial to recognize the symptoms specific to each age group for appropriate care and treatment. For any persistent or severe symptoms, a consultation with a dermatologist is recommended.
When to see your doctor
Eczema can often be managed with over-the-counter treatments and home remedies, but there are situations where medical intervention is necessary. It’s crucial to recognize when professional help is needed. Here are signs that it’s time to consult a doctor:
- Persistent or Worsening Symptoms: If eczema does not improve after a couple of weeks of self-care or over-the-counter treatments, or if it worsens, a doctor should be consulted.
- Intense Itching: If itching becomes so severe that it disrupts daily activities or sleep, it’s time to seek medical advice.
- Signs of Infection: Indications can include increased redness, warmth, pus, yellowish crusts, or if the affected skin area feels hot. Infections require prompt treatment.
- Eczema on the Face or Genitals: These areas can be more challenging to treat on your own and may need specialized care.
- Interference with Daily Activities: If eczema symptoms are causing distractions in work, school, or daily routines, it’s essential to get a professional assessment.
- Unsure of Diagnosis: Eczema can sometimes be mistaken for other skin conditions. If there’s uncertainty about the diagnosis, always consult a dermatologist.
- Treatment Side Effects: If there are any unusual reactions to treatments or creams, such as increased burning or redness, a doctor should be informed.
Remember, while mild eczema can often be managed at home, persistent or severe cases require a doctor’s expertise. It’s always better to be cautious and get a professional opinion to ensure the best care for your skin.

Causes
The exact causes of eczema remain unclear, but it’s believed to develop due to a combination of genetic and environmental factors4. Here are some of the key factors associated with eczema:
- Genetic Predisposition: Individuals with a family history of eczema, allergies, hay fever, or asthma are more likely to develop eczema. Certain genes can make the skin more susceptible to irritants and allergens.
- Impaired Skin Barrier: Eczema sufferers often have a compromised skin barrier, making it easier for moisture to be lost and allergens to penetrate the skin, leading to dryness and inflammation.
- Immune System Overactivity: An overactive immune response to irritants can lead to the skin inflammation seen in eczema.
- Environment: Living in urban areas or places with higher levels of pollution can increase the risk. Additionally, colder climates with low humidity can dry out the skin, exacerbating the condition.
- Allergens: Exposure to certain allergens, like dust mites, pollen, mold, or pet dander, can trigger or worsen eczema symptoms in some individuals.
- Irritants: Everyday products such as soaps, detergents, shampoos, and even certain fabrics can irritate the skin and trigger eczema flare-ups.
- Stress: While not a direct cause, stress is known to exacerbate eczema symptoms in many individuals.
- Hormones: Changes in hormone levels, such as those experienced during menstruation or pregnancy, can trigger eczema in some individuals.
It’s important to remember that the exact cause of eczema may differ from one person to another. While some may be genetically predisposed, others might experience flare-ups primarily due to environmental triggers. A thorough evaluation by a dermatologist can help identify the potential causes and contributing factors specific to each individual.
Risk Factors
Eczema can affect anyone, but certain factors may increase an individual’s likelihood of developing this skin condition. Recognizing these risk factors can aid in prevention and management.
- Family History: Individuals with a family history of eczema, allergies, or asthma are at an increased risk of developing eczema.
- Asthma and Allergies: Those with asthma or allergic conditions such as hay fever, allergic rhinitis, or food allergies have a higher propensity to develop eczema.
- Early Childhood: Infants and young children are at higher risk due to their developing immune systems and skin barrier function.
- Occupational Hazards: Individuals in professions that expose them to irritants or allergens, such as healthcare, cleaning, or hairdressing, may be at an increased risk.
- Geographical Location: People living in urban areas or places with lower humidity levels are more likely to develop eczema.
- Skin Barrier Function: An impaired skin barrier allows moisture to escape and can let harmful substances in, increasing the risk of eczema.
- Immune System Disorders: Conditions that affect the immune system might also increase the risk of eczema.
- Chronic Stress: Persistent stress can weaken the immune system and may potentially exacerbate eczema symptoms.
Understanding one’s risk factors doesn’t necessarily predict the onset of eczema but provides insight into the potential for its development. If you or a loved one exhibits signs of eczema, especially with multiple risk factors present, it’s advisable to consult a dermatologist for an accurate diagnosis and management plan.
Food Triggers
Certain foods can trigger eczema flare-ups in some individuals, especially those with food sensitivities or allergies. Being aware of common food triggers and understanding why they may exacerbate eczema is crucial for the effective management of the condition.
- Dairy Products, such as milk, cheese, and butter, can trigger inflammatory responses due to the proteins they contain.
- Eggs, especially egg whites, can provoke skin irritation as the proteins in eggs might cause allergic reactions.
- Nuts and Seeds, like almonds and peanuts, might exacerbate eczema because their proteins and oils can trigger allergic responses in certain individuals.
- Soy Products, including tofu and soy milk, can be problematic for some people due to the allergic reactions soy proteins might cause.
- Wheat-based foods, including bread and pasta, can irritate the skin of gluten-sensitive individuals because of the immune response to gluten.
- Citrus Fruits, such as oranges and lemons, might lead to flare-ups in some due to their acidity and citrus proteins.
- Seafood, including certain fish and shellfish, can be a trigger for those allergic to seafood proteins.
Awareness of these food triggers and potentially limiting or eliminating them from the diet can help manage eczema symptoms more effectively.

Foods That Help Manage Eczema
Certain foods have properties that may benefit individuals with eczema by reducing inflammation, bolstering the immune system, or maintaining skin health. Incorporating these into one’s diet might provide relief from symptoms.
- Fatty Fish: Salmon, mackerel, sardines, and herring are rich in omega-3 fatty acids, and known for their anti-inflammatory properties.
- Flaxseeds: Another excellent source of omega-3s, they can be added to smoothies, oatmeal, or baked goods.
- Probiotics: Yogurt, kefir, sauerkraut, and other fermented foods can improve gut health and boost the immune system.
- Fruits and Vegetables: Blueberries, cherries, spinach, and kale contain antioxidants and flavonoids that may help reduce inflammation.
- Bone Broth: Rich in collagen, which can support skin health and elasticity.
- Zinc-rich Foods: Pumpkin seeds, cashews, and chickpeas can promote skin healing.
- Turmeric: Contains curcumin, known for its potent anti-inflammatory and antioxidant properties.
Including beneficial foods in one’s diet can be a natural way to support skin health and potentially reduce eczema symptoms. However, always remember that individual responses to foods can vary. What works for one person might not work for another. It’s always a good idea to consult with a nutritionist or healthcare provider when making significant dietary changes, especially when aiming to manage a health condition.

Diagnosis
Diagnosing eczema involves a combination of physical examination, medical history evaluation, and sometimes specific tests. Early diagnosis can aid in better management and treatment of the condition.
- Physical Examination: A dermatologist or primary care doctor will examine the affected skin areas to identify characteristic signs of eczema.
- Medical History: Understanding a patient’s medical and family history can offer clues. The doctor might inquire about any family members with eczema, allergies, or similar conditions.
- Patch Testing: If contact dermatitis is suspected, a doctor may recommend patch testing. This involves applying small amounts of potential irritants to the skin to see if there’s a reaction.
- Allergy Testing: Blood tests or skin prick tests can help identify allergens that may be triggering or exacerbating the eczema.
- Skin Biopsy: In rare cases, if the diagnosis is unclear, a small skin sample might be taken to examine under a microscope.
Accurate diagnosis is paramount for effective eczema management. If you suspect you have eczema or experience persistent skin issues, it’s crucial to see a healthcare professional for a proper evaluation and guidance on managing the condition.
Treatment
Eczema treatment aims to control symptoms, prevent flare-ups, and maintain skin health. The right treatment approach can significantly enhance the quality of life for individuals with eczema.
- Topical Treatments: Directly applied to the skin, these provide immediate relief to the affected areas, helping in reducing inflammation, and itching, and promoting skin healing.
- Steroid Creams and Ointments: Used to alleviate inflammation and irritation.
- Calcineurin Inhibitors: A non-steroidal treatment that manages inflammation.
- Emollients: Moisturizers are essential for hydrating and forming a protective skin barrier.
- Steroid Creams and Ointments: Used to alleviate inflammation and irritation.
- Medication: These oral or injectable drugs address internal causes or severe symptoms of eczema5.
- Antihistamines: Prescribed to reduce itching, especially at nighttime.
- Oral Corticosteroids: Tackle severe inflammation cases.
- Immunosuppressants: Help in modulating an overactive immune response.
- Antihistamines: Prescribed to reduce itching, especially at nighttime.
- Phototherapy: This involves the exposure of skin to specific ultraviolet light wavelengths under medical guidance, benefiting those with moderate to severe eczema.
- UVA/UVB Therapy: Reduces itching, and inflammation, and helps in increasing vitamin D production.
- UVA/UVB Therapy: Reduces itching, and inflammation, and helps in increasing vitamin D production.
- Biologic Drugs: Advanced medications specifically designed to target and interrupt certain pathways in the immune system.
- Dupilumab: An example that targets specific immune pathways, offering relief when other treatments fall short.
- Dupilumab: An example that targets specific immune pathways, offering relief when other treatments fall short.
- Skincare Routine: Adopting a daily regimen of cleansing and moisturizing with products suitable for sensitive skin helps in maintaining skin health.
- Gentle Cleansers: Used to clean without stripping skin’s natural oils.
- Therapeutic Moisturizers: Provide prolonged hydration and prevent dryness.
- Gentle Cleansers: Used to clean without stripping skin’s natural oils.
- Stress Management and Lifestyle Adjustments: Managing everyday stress can significantly reduce eczema flare-ups.
- Mindfulness and Meditation: Techniques that help in relaxation and mental well-being.
- Yoga: A physical activity known to reduce stress and improve skin health.
- Mindfulness and Meditation: Techniques that help in relaxation and mental well-being.
By integrating these treatments based on individual needs and under professional guidance, eczema sufferers can expect improved skin health and a better quality of life.
Complications
While eczema primarily affects the skin, if not managed effectively, it can lead to various complications, impacting both physical health and quality of life.
- Skin Infections: Persistent scratching or broken skin can introduce bacteria, leading to infections like impetigo.
- Eye Complications: Eczema around the eyes can lead to conditions such as blepharitis or conjunctivitis. In severe cases, it could affect vision.
- Sleep Disturbances: The constant itchiness and discomfort can severely impact sleep quality, leading to fatigue and other health issues.
- Asthma and Allergies: Individuals with eczema are more likely to develop asthma and allergies due to the interconnectedness of immune responses.
- Mental Health Issues: The chronic nature of eczema and its visible manifestations can contribute to anxiety, depression, or self-esteem issues.
- Hand Eczema6: Eczema on the hands can be debilitating, affecting one’s ability to carry out daily tasks.
Early intervention and consistent management of eczema can significantly reduce the risk of these complications.
Prevention
While it’s challenging to prevent eczema entirely, especially if one is genetically predisposed, there are several measures to reduce the frequency and severity of flare-ups.
- Moisturize Regularly: Keeping skin hydrated with fragrance-free moisturizers can help maintain its barrier and reduce dryness.
- Avoid Known Allergens: Identify and steer clear of allergens, such as certain foods, pollens, or pet dander, that can instigate flare-ups.
- Maintain a Stable Environment: Extreme temperatures and humidity can exacerbate eczema. Using a humidifier in dry environments and avoiding sudden temperature changes can help.
- Choose Mild Soaps and Detergents: Opt for fragrance-free, hypoallergenic products, and ensure you rinse them off thoroughly.
- Wear Soft, Breathable Fabrics: Natural fabrics like cotton can prevent irritation. Avoid rough, scratchy fibers and tight clothing.
- Manage Stress: Stress can be a trigger for some individuals. Finding coping mechanisms, like meditation or counseling, can be beneficial.
- Avoid Scratching: Scratching can worsen symptoms and lead to infections. Keeping nails short and using cold compresses can help manage the itch.
By proactively adopting these preventive measures, individuals can effectively reduce the chances of eczema flare-ups and maintain healthier skin.

Final Thoughts
Eczema, a persistent skin condition, requires a well-rounded understanding for effective management. Recognizing individual triggers, be they environmental allergens or certain foods, and seeking professional guidance are essential steps toward managing symptoms.
While there isn’t a one-size-fits-all solution, a combination of medical treatments, lifestyle modifications, and proactive management can significantly improve the quality of life for individuals with eczema.
Continuous research and advancements in treatment offer hope for even more effective management solutions in the near future.
FAQs
Sources
- “Eczema (Atopic Dermatitis): Causes, Treatment & Symptoms.” Cleveland Clinic, 1 Oct. 2023, my.clevelandclinic.org/health/diseases/9998-eczema#diagnosis-and-tests. Accessed 1 Oct. 2023. ↩︎
- National Eczema Association. “Eczema Symptoms & Causes.” National Eczema Association, 2017, nationaleczema.org/eczema/. Accessed 1 Oct. 2023. ↩︎
- “Eczema: Symptoms, Treatment, Causes, and Types.” Www.medicalnewstoday.com, 1 June 2020, www.medicalnewstoday.com/articles/14417#symptoms. Accessed 1 Oct. 2023. ↩︎
- Mayo Clinic. “Atopic Dermatitis (Eczema) – Symptoms and Causes.” Mayo Clinic, 2020, www.mayoclinic.org/diseases-conditions/atopic-dermatitis-eczema/symptoms-causes/syc-20353273. Accessed 1 Oct. 2023. ↩︎
- —. “Eczema.” WebMD, 14 July 2023, www.webmd.com/skin-problems-and-treatments/eczema/atopic-dermatitis-eczema. Accessed 1 Oct. 2023. ↩︎
- “7 Types of Eczema: Symptoms, Causes, and Pictures.” Healthline, 1 Oct. 2023, www.healthline.com/health/types-of-eczema#hand-eczema. Accessed 1 Oct. 2023. ↩︎