Allergies. We’ve all heard of them, and many of us have experienced the sneezing, itching, and discomfort firsthand. These are just a few inconveniences that significantly impact our daily lives because of allergies. But by understanding their root causes and manifestations, we can strategize more effectively.
Picture a world where you’re better equipped to manage these irritants, turning what once was dread into knowledge-powered confidence. Read on and let’s unpack the world of allergies together.
What is Allergies?
Allergies are a heightened immune response to specific substances, termed allergens, which are typically harmless to the majority of individuals1. This reaction occurs when an allergic person’s immune system mistakenly identifies the allergen as a threat, leading to symptoms that can range from mild discomforts, such as itching or sneezing, to severe, potentially life-threatening conditions like anaphylaxis2.
Common Allergens
Common allergens are substances that can trigger allergic reactions in sensitive individuals. Here are some of the most prevalent:
- Airborne Allergens:
- Pollen: Tiny particles released by trees, grasses, and weeds.
- Animal Dander: Small flecks of skin shed by animals such as cats, dogs, rodents, and birds.
- Dust Mites: Microscopic creatures that live in household dust.
- Mold: Fungi that release tiny spores that can be inhaled.
- Pollen: Tiny particles released by trees, grasses, and weeds.
- Food Allergens:
- Peanuts: Often cause severe allergic reactions in some people.
- Tree Nuts: Includes almonds, walnuts, and cashews.
- Wheat: Present in many foods and can trigger reactions in those with wheat allergies or celiac disease.
- Soy: Used in many processed foods and can be an allergen for some.
- Fish and Shellfish: Some individuals are allergic to certain fish or shellfish, like shrimp, crabs, and lobsters.
- Eggs: A common allergen, especially in children.
- Milk: Another common allergen in children, though many outgrow this allergy.
- Peanuts: Often cause severe allergic reactions in some people.
- Insect Venom:
- Bees: Venom from bee stings can cause allergic reactions.
- Wasps: Including yellow jackets and hornets.
- Bees: Venom from bee stings can cause allergic reactions.
- Medications:
- Penicillin: An antibiotic that some people are allergic to.
- Other Medications: Various other drugs can also be allergens for some individuals.
- Penicillin: An antibiotic that some people are allergic to.
- Contact Allergens:
- Latex: This can cause allergic reactions in some individuals when they come into contact with it.
- Chemicals: Found in cosmetics, hair dye, or certain plants can also lead to contact dermatitis in sensitive individuals.
- Latex: This can cause allergic reactions in some individuals when they come into contact with it.
Understanding and avoiding these common allergens, if one is allergic, is essential for preventing allergic reactions.

Signs and Symptoms of Allergies
Allergic reactions manifest in various ways, depending on the type of allergen and the individual’s sensitivity3. Here are some of the most common signs and symptoms associated with allergies:
- Hay Fever (Allergic Rhinitis)4:
- Sneezing
- Itching of the nose, eyes, or roof of the mouth
- Runny, stuffy nose
- Watery, red, or swollen eyes (conjunctivitis)
- Sneezing
- Food Allergies:
- Tingling or itching in the mouth
- Swelling of the lips, tongue, face, or throat
- Hives (itchy red spots on the skin)
- Anaphylaxis (a severe, potentially life-threatening allergic reaction)
- Tingling or itching in the mouth
- Insect Sting Allergies:
- Localized swelling and redness at the sting site
- Itching or hives all over the body
- Cough, chest tightness, wheezing, or shortness of breath
- Anaphylaxis
- Localized swelling and redness at the sting site
- Medication Allergies:
- Skin rash or hives
- Itchy skin
- Swelling of the face or extremities
- Wheezing or difficulty breathing
- Anaphylaxis
- Skin rash or hives
- Contact Dermatitis (Allergic Skin Reaction):
- Redness and rash
- Itching or burning sensation
- Blisters that may weep or ooze, in severe cases
- Flaking or peeling skin
- Redness and rash
- Anaphylaxis: A severe and rapid allergic reaction that can affect multiple systems in the body. Symptoms can include:
- Difficulty breathing due to swelling of the throat
- Rapid, weak pulse
- Drop in blood pressure
- Skin rash
- Nausea, vomiting, or diarrhea
- Loss of consciousness
- Difficulty breathing due to swelling of the throat
It’s crucial to recognize and respond promptly to allergic reactions, especially anaphylaxis, as it can be life-threatening. Those with known severe allergies often carry an epinephrine auto-injector (e.g., EpiPen) to treat anaphylactic reactions. If someone is experiencing symptoms of anaphylaxis, it’s imperative to seek emergency medical attention immediately.

Risk Factors
Allergic reactions affect individuals differently, and while anyone can develop allergies, certain factors increase the risk. Recognizing these risk factors can aid in early detection and management of allergic responses.
1. Family History
- Genetics plays a significant role in allergies. If one’s parents or siblings have allergies, they are more likely to develop them. This includes conditions like hay fever, hives, or eczema.
2. Age
- Children are more susceptible to allergies because their immune systems are still developing. While some outgrow these allergies, others carry them into adulthood.
3. Asthma and Other Allergic Conditions
- Individuals with conditions like asthma or other allergies are more likely to develop additional allergic reactions. For instance, someone with hay fever might later develop a food allergy.
4. Previous Allergic Reactions
- Experiencing an allergic reaction increases the likelihood of subsequent reactions. These can sometimes be more severe than the initial reaction.
5. Environmental Exposures
- Being continuously exposed to allergens, especially at a younger age, may increase the risk of allergies. This includes prolonged exposure to pollutants or certain chemicals.
6. Occupation
- Some professions might expose individuals to allergens or irritants more frequently, increasing the risk. For example, bakers might develop wheat allergies, and healthcare workers might develop latex allergies.
Being aware of the risk factors associated with allergies allows for better preparedness and preventive actions. Individuals should always consult with healthcare professionals if they believe they are at a heightened risk, ensuring they receive the necessary guidance and support.
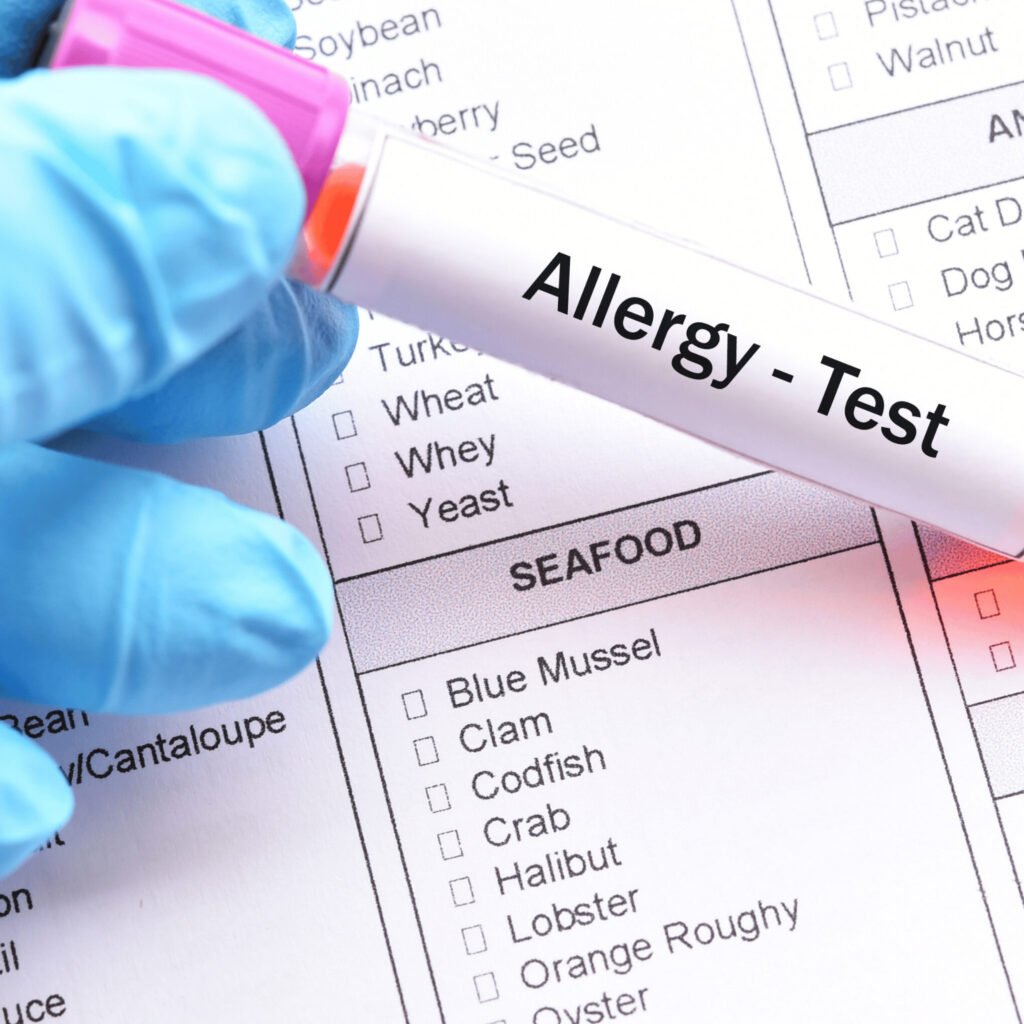
Diagnoses
Diagnosing allergies is essential to ensure appropriate management and treatment. A combination of a patient’s medical history, physical examination, and specific tests can identify the exact cause of allergic reactions. Here are the ways of diagnosing allergies:
1. Medical History and Physical Examination
- A detailed discussion with the patient about their symptoms, their frequency, and possible triggers provides initial insights. Often, patterns in symptom emergence can point toward specific allergens.
2. Skin Prick Test (SPT)5
- This is one of the most common methods of allergy testing. Small amounts of suspected allergens are pricked into the surface of the skin using a tiny device. The appearance of a raised, red bump indicates a potential allergy to that substance.
3. Blood Tests
- A blood test, often called an IgE test, measures the amount of allergy-causing antibodies in the bloodstream. It’s particularly useful when skin tests might be unsafe or could produce inaccurate results.
4. Challenge Testing
- Under careful supervision, a patient consumes or inhales a small amount of the suspected allergen. This method is more common for potential food or medication allergies and is done only when strictly necessary due to the risk of a severe reaction.
5. Patch Testing
- Used predominantly for diagnosing contact dermatitis, allergenic substances are applied on patches, which are then placed on the skin. After 48 hours, the skin is examined for reactions.
For complex cases or rare allergens, seeing an allergist immunologist, or specialist in allergies, might be required. These experts possess the knowledge and tools to offer a more in-depth diagnosis.
Treatment For Allergies
Allergies can be disruptive and sometimes life-threatening. Here’s a comprehensive approach to effectively manage symptoms and reduce allergen reactions:
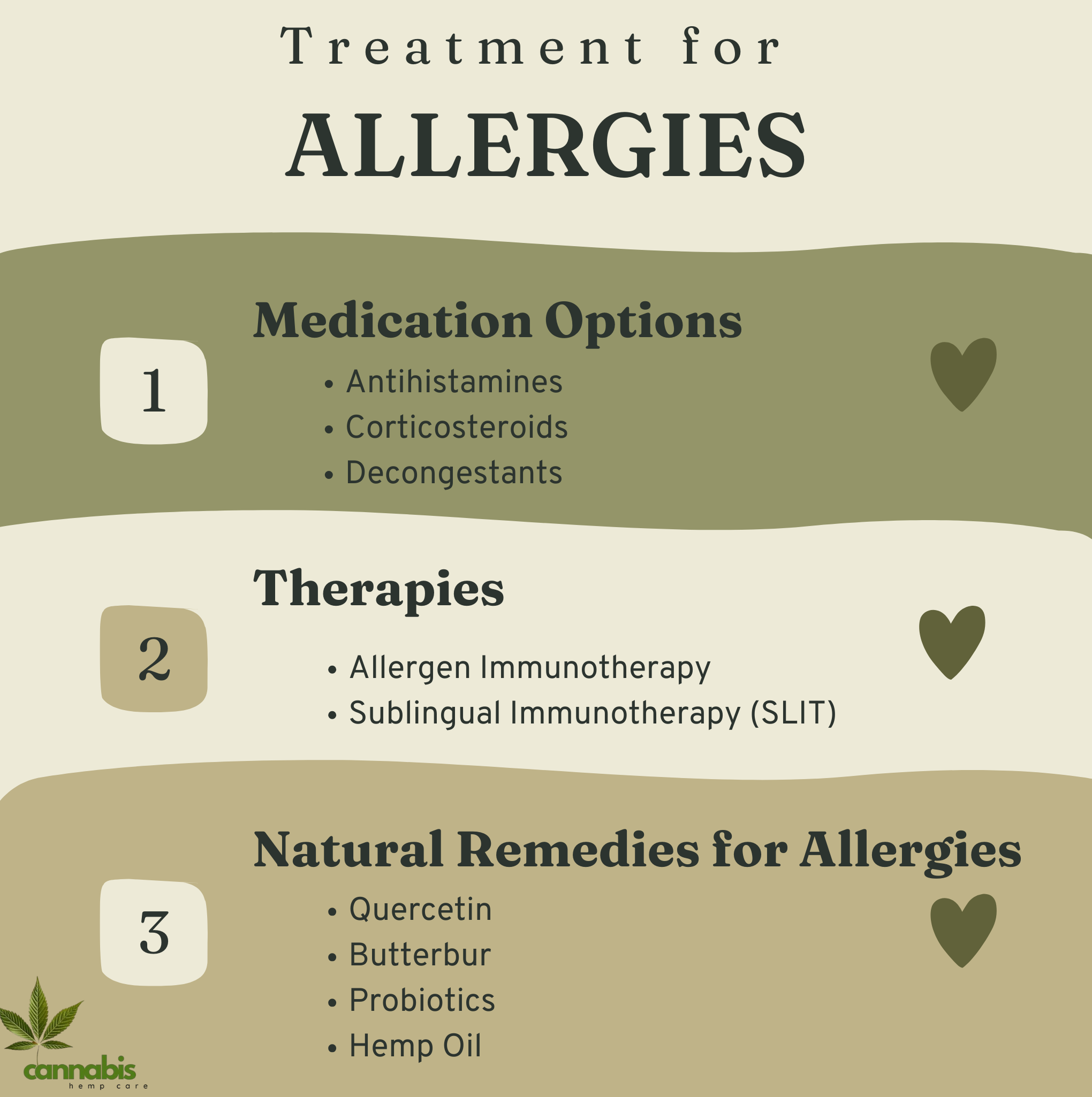
Medication Options
Antihistamines
- These counteract the effects of histamine, the compound that causes allergy symptoms. Examples include cetirizine, fexofenadine, and loratadine. They can provide relief from sneezing, itching, and runny noses.
Corticosteroids
- Administered as nasal sprays, inhalers, or oral medications, corticosteroids reduce inflammation and allergy symptoms. Examples are fluticasone, budesonide, and mometasone.
Decongestants
- Used to provide short-term relief from nasal congestion. Examples include pseudoephedrine and phenylephrine. They should be used cautiously, especially among those with heart conditions.
Therapies
Allergen Immunotherapy
- Commonly known as allergy shots, this involves regular injections of gradually increasing quantities of the allergen. Over time, this can reduce the severity of allergic reactions.
Sublingual Immunotherapy (SLIT)
- Instead of shots, small doses of the allergen are placed under the tongue. This method is especially common for pollen and dust mite allergies.
Natural Remedies for Allergies
Quercetin
- Found in fruits and vegetables like apples and onions, quercetin is a natural antihistamine that can help reduce allergy symptoms.
Butterbur
- A herb that can effectively treat hay fever without the drowsiness caused by antihistamines.
Probiotics
- These beneficial bacteria can modulate the immune system, potentially reducing allergic reactions. They can be found in yogurt, kefir, and specific supplements.
- Hemp oil contains omega fatty acids that reduce inflammation, often associated with allergies. Its anti-inflammatory properties can help alleviate allergy symptoms.
Food That Helps Manage Allergy
Certain foods, rich in vitamins, minerals, and other beneficial compounds, can aid in bolstering the immune system and possibly reducing allergy symptoms. Incorporating these foods into one’s diet can help in creating a balance and ensuring overall well-being.
- Found in fatty fish like salmon, walnuts, and flaxseeds, omega-3 fatty acids have anti-inflammatory properties that may help reduce allergic reactions.
2. Probiotics
- Foods rich in probiotics, such as yogurt, kefir, and fermented foods, can help balance the gut microbiota. A healthy gut can support a robust immune system and potentially reduce allergy symptoms.
3. Vitamin C
- Present in citrus fruits, strawberries, and bell peppers, Vitamin C is an antioxidant that supports the immune system and may help clear out histamines, thus reducing allergy symptoms.
4. Quercetin
- Found in apples, berries, onions, and black tea, quercetin is a flavonoid that has shown potential in stabilizing mast cells, which release histamine and other inflammatory signals during allergic reactions.
5. Pineapple
- This tropical fruit contains bromelain, an enzyme that can help reduce allergic reactions’ severity by breaking down proteins causing inflammation in the body.
6. Turmeric
- Renowned for its anti-inflammatory properties due to its active component, curcumin. Adding turmeric to dishes or consuming it as a supplement may help in reducing allergy symptoms.
7. Green Tea
- Contains a compound called epigallocatechin gallate (EGCG), which has been studied for its potential to reduce allergy symptoms. Drinking green tea regularly might offer protective benefits against allergens.
While specific foods possess properties that can aid in allergy relief, it’s crucial to consult with a healthcare professional or nutritionist before making significant dietary changes, especially for those with known food allergies or dietary restrictions.
Prevention
Allergies, while often genetic or environmentally predisposed, can sometimes be managed or even prevented through certain measures. Proper precautions can limit exposure and reduce the severity of allergic reactions.
Avoid Known Triggers
The most effective way to prevent an allergic reaction is to avoid known allergens. This may involve:
- Staying indoors during peak pollen seasons.
- Using allergy-proof covers for pillows and mattresses to keep out dust mites.
- Avoiding foods or medications that have previously caused an allergic reaction.
Keep a Diary
Maintaining a record of activities, foods consumed, and the onset of symptoms can be beneficial. This diary can help in:
- Identifying potential new allergens.
- Recognizing patterns or trends related to allergic reactions.
Wear a Medical Alert Bracelet
For individuals with severe allergies, especially those at risk of anaphylaxis, wearing a medical alert bracelet can be lifesaving. It:
- Alerts healthcare professionals and the public about the individual’s allergy.
- Ensures prompt and appropriate medical attention in emergencies.
Environmental Control
Reducing exposure to airborne allergens can prevent symptoms. This includes:
- Using high-efficiency particulate air (HEPA) filters in homes.
- Regular cleaning and vacuuming to reduce pet dander and dust.
While it’s challenging to completely avoid allergens, understanding and implementing these preventive measures can significantly mitigate the risk and severity of allergic reactions.
Complications
Allergies, while often manageable, can lead to complications if not properly addressed. Recognizing potential complications can aid in early detection and intervention, minimizing risks and enhancing the quality of life for affected individuals.
Anaphylaxis
The most severe form of allergic reaction, anaphylaxis can be life-threatening if not treated immediately6. It can be triggered by certain foods, insect stings, and medications, among other allergens. Symptoms include:
- Loss of consciousness
- Severe shortness of breath
- Rapid, weak pulse
Asthma
Allergic reactions can aggravate or even initiate asthma symptoms. This condition, known as allergy-induced asthma, results in:
- Difficulty breathing
- Chest tightness
- Chronic cough
Sinusitis
Chronic allergic reactions, especially hay fever, can lead to sinusitis – an inflammation or swelling of the tissue lining the sinuses. Symptoms encompass:
- Nasal congestion
- Thick yellow or green nasal discharge
- Reduced sense of smell and taste
Ear or Lung Infections
Individuals with allergies, particularly hay fever, are at a higher risk of developing ear or lung infections. The inflammation and mucus production can lead to bacterial growth and subsequent infections.
Allergies, while common, can lead to more severe health complications if not monitored and managed. It is vital for individuals with allergies to stay informed, maintain regular check-ups, and seek medical attention if they notice any exacerbation or new symptoms. This proactive approach can help prevent complications and ensure a better quality of life.
Prognosis of Allergies
Allergies, while chronic in nature, often exhibit varied courses over an individual’s lifetime. The prognosis, or long-term outlook, largely depends on the type of allergy, its severity, and the management approaches taken.
Factors Influencing Prognosis
Type of Allergen
- Some allergies, such as those to milk or eggs, are often outgrown in childhood. Conversely, allergies like those to peanuts or shellfish tend to persist throughout life.
Early Diagnosis and Intervention
- Timely detection and management of allergies can significantly improve the long-term outlook, potentially reducing the severity of reactions in the future.
Severity of Initial Reaction
- Individuals who experience more severe initial reactions may be at a higher risk for severe future reactions, making vigilance and preventative measures even more crucial.
Management and its Impact on Prognosis
Allergen Avoidance
- The simplest and most effective approach. By understanding and avoiding specific triggers, one can substantially reduce the frequency and severity of allergic reactions.
Medication and Therapy
- Regular use of prescribed antihistamines, corticosteroids, or immunotherapy can control symptoms and might improve tolerance to certain allergens over time.
Lifestyle Adjustments
- Maintaining a clean environment, adhering to dietary restrictions, and being prepared with emergency interventions (like epinephrine auto-injectors) can drastically affect prognosis by preventing unintentional exposures and swift management of reactions.
While allergies present lifelong challenges for many, the prognosis is generally favorable with appropriate knowledge, management, and precautions. Continued research and advancements in allergy care promise even brighter prospects for those affected.
Living with allergies
Living with allergies can be challenging, but with the right strategies and knowledge, individuals can lead a fulfilling and symptom-free life. Understanding how to navigate daily life while managing allergies is crucial for overall well-being.
Daily Management
For many, daily management involves avoiding known allergens, taking prescribed medications, and staying vigilant about potential triggers7. This might include:
- Checking weather reports for pollen counts
- Using allergen-proof bed covers
- Regularly cleaning living spaces to minimize allergens
Dietary Adjustments
For those with food allergies8:
- Reading food labels becomes essential
- Cooking at home can offer more control over ingredients
- Carrying an EpiPen or similar device is crucial in case of accidental exposure
Social Considerations
Interacting with others can pose challenges for those with allergies:
- It’s important to communicate with friends and family about your allergies, especially food allergies, to prevent accidental exposure.
- Planning ahead when dining out or traveling is crucial, such as checking restaurant menus or notifying flight attendants about your allergies.
Emotional Well-being
Living with allergies can also have emotional implications9:
- Anxiety about exposure can be common, especially in public spaces or unfamiliar environments.
- Seeking support groups or counseling can be beneficial for coping and emotional well-being.
While living with allergies requires diligence and adaptation, it doesn’t mean compromising on the quality of life. By being informed, proactive, and seeking support when needed, individuals with allergies can lead a full and enriching life, minimizing disruptions and maximizing enjoyment.
When to see a doctor?
Recognizing when allergies shift from mild discomfort to a potential health risk is critical. Timely consultation with a healthcare provider can ensure proper treatment, prevent complications, and enhance the quality of life.
Initial Symptoms
The onset of unfamiliar or severe allergy symptoms necessitates medical attention:
- Persistent sneezing, coughing, or nasal congestion
- Itching or hives that don’t improve with over-the-counter treatments
Food Allergy Reactions
If consuming certain foods results in:
- Tingling or swelling in the mouth
- Difficulty breathing or swallowing
- Sudden onset of hives or itching It’s crucial to consult a doctor.
Severe Allergic Reactions (Anaphylaxis)
For reactions that may be life-threatening:
- Difficulty breathing
- Rapid or weak pulse
- Sudden drop in blood pressure
- Loss of consciousness Immediate medical attention is imperative. Call emergency services or head to the nearest emergency room.
Chronic or Recurring Symptoms
If allergy symptoms:
- Persist for several weeks
- Disrupt daily activities or sleep
- Are not alleviated by over-the-counter remedies A visit to a specialist, like an allergist or immunologist, might be necessary.
It’s essential to listen to one’s body and recognize signs that require medical intervention. Consulting a doctor or specialist when experiencing significant allergy symptoms can lead to effective management strategies and a better understanding of individual triggers, ensuring a healthier, more comfortable life.

Final Thoughts
Allergies, whether mild or severe, can significantly impact an individual’s quality of life. It is crucial to recognize triggers, understand symptom management, and seek medical guidance when necessary. Staying informed and proactive can make a significant difference in managing and potentially alleviating allergy symptoms.
FAQs
Sources
- “Allergies Explained – Better Health Channel.” Www.betterhealth.vic.gov.au, 2 Oct. 2023, www.betterhealth.vic.gov.au/health/conditionsandtreatments/allergies. Accessed 2 Oct. 2023. ↩︎
- “Allergy.” Medlineplus.gov, National Library of Medicine, 2019, medlineplus.gov/allergy.html Accessed 2 Oct. 2023. ↩︎
- “Allergies – Types, Risk Factors, Complications, and Prevention | Everyday Health.” EverydayHealth.com, 31 May 2019, www.everydayhealth.com/allergies/ Accessed 2 Oct. 2023. ↩︎
- “Allergies – Symptoms and Causes.” Mayo Clinic, 5 Aug. 2022, www.mayoclinic.org/diseases-conditions/allergies/symptoms-causes/syc-20351497#:~:text=Allergies%20occur%20when%20your%20immune Accessed 2 Oct. 2023. ↩︎
- NHS Choices. “Allergies.” NHS, 2019, www.nhs.uk/conditions/allergies/. Accessed 2 Oct. 2023. ↩︎
- “Allergies Overview: Symptoms, Treatments, and More.” Healthline, 5 June 2018, www.healthline.com/health/allergies#takeaway Accessed 2 Oct. 2023. ↩︎
- “Allergies.” Asthma & Allergy Foundation of America, 7 Oct. 2023, aafa.org/allergies/. Accessed 7 Oct. 2023. ↩︎
- “Food Allergy 101 – Basics of Food Allergies | FARE.” Food Allergy Research & Education, 2020, www.foodallergy.org/living-food-allergies/food-allergy-essentials/food-allergy-101. Accessed 7 Oct. 2023. ↩︎
- Allergy UK. “Allergy UK.” Allergyuk.org, 2019, www.allergyuk.org/. Accessed 7 Oct. 2023. ↩︎