Every new parent cherishes the moments of caressing their infant’s soft, delicate skin. But those flaky, yellowish patches on their little head? That’s a surprise many don’t anticipate.
Welcome to the world of cradle cap, a frequent guest in the early months of parenthood. Although it may initially raise eyebrows, a deeper understanding can alleviate any unease.
So, take a pause, just as you would for a baby’s first smile or giggle, and journey with us through the nuances of cradle cap. Consider this your guide to navigating yet another intriguing chapter of early parenthood.
What is a Cradle Cap?
Cradle cap, or pityriasis capitis is a common, harmless skin condition in infants. Medically, it’s known as infantile seborrheic dermatitis1. While its exact cause is unclear, it may be related to the production of excess oil in the skin’s oil glands and hair follicles.
Cradle cap typically appears between the ages of one and three months. Around 70% of infants under 3 months old develop cradle caps. In most cases, it disappears after a year2. However, some babies develop it around 1 or 2 years old. The condition is recognizable by the presence of:
- Yellowish or brownish scales that can look crusty or greasy.
- Mild redness on the affected scalp.
- Occasionally, a mild odor.
Although it’s most commonly found on the scalp, this can also appear on other areas such as the eyebrows, eyelids, ears, nose, and even the groin3.
Causes of Cradle Cap
Infantile seborrheic dermatitis is a skin condition that primarily affects infants. Though its exact cause remains a subject of ongoing research, several prominent factors have been identified.
1. Overactive Sebaceous Glands
Babies have high levels of maternal hormones in their bloodstream for several months after birth, which can cause the oil-producing sebaceous glands in the skin to produce more oil, leading to cradle caps. In infants:
- Elevated maternal hormones persist in the baby’s system for several months post-birth.
- These hormones stimulate the sebaceous glands, leading them to produce an excess of sebum.
- The surplus of sebum on the baby’s scalp is believed to be a significant contributor to the onset of cradle cap.
2. Fungal Growth
The skin naturally hosts a variety of microorganisms, including the yeast Malassezia.
- In environments with high sebum production, Malassezia tends to multiply more rapidly.
- This yeast (fungus) called Malassezia can grow in the sebum along with bacteria, and this might play a role in the development of cradle cap4.
3. External Irritants
A baby’s skin is sensitive and can react to various external products.
- Some shampoos, lotions, or detergents contain ingredients that might irritate an infant’s delicate skin.
- This irritation can either instigate or exacerbate cradle cap symptoms.
Understanding these causes can aid caregivers in preventing potential triggers and managing existing symptoms more effectively.
Symptoms of Cradle Cap
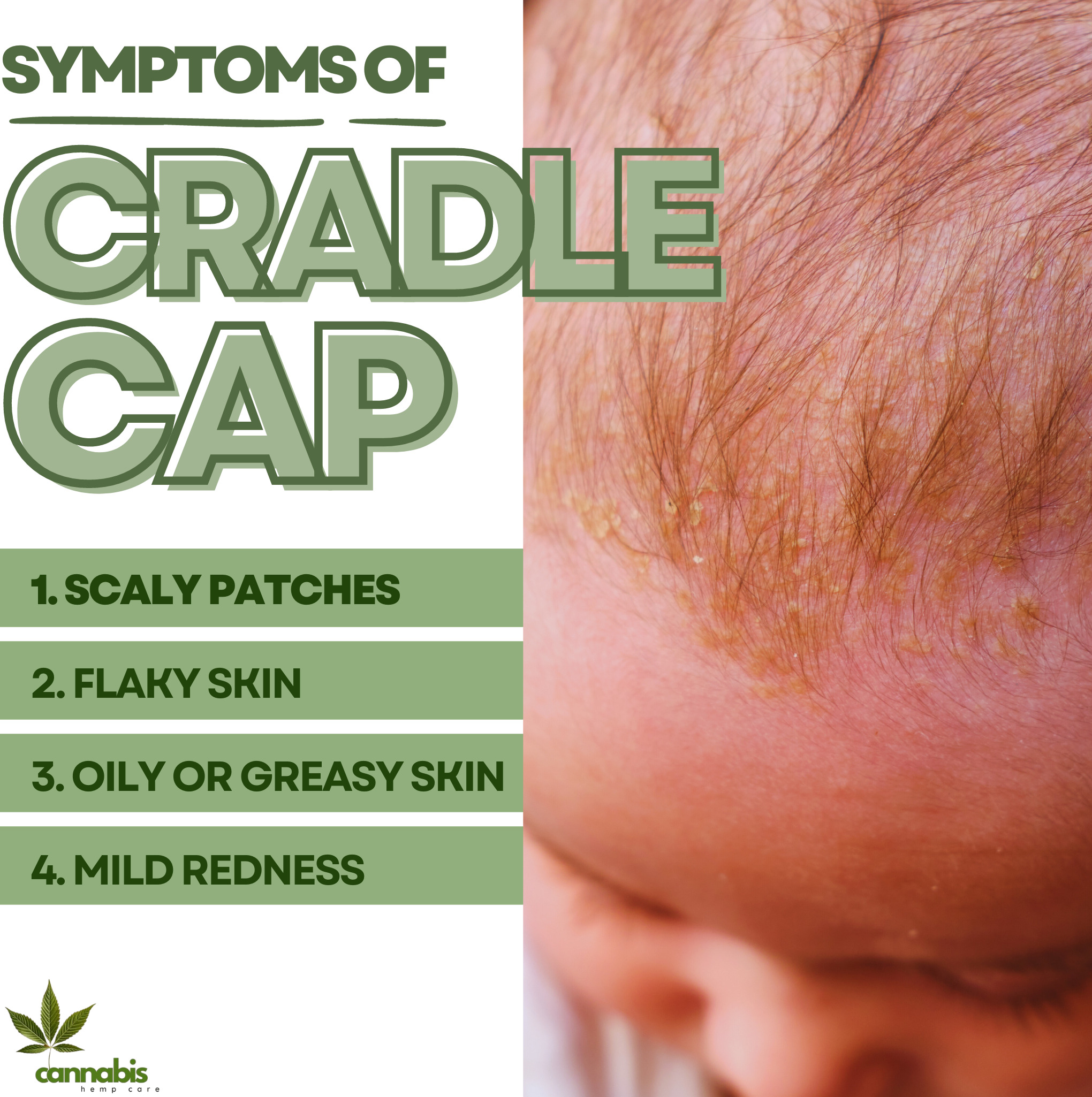
Recognizing these symptoms can aid in early diagnosis and management.
1. Scaly Patches
One of the most identifiable signs of cradle cap is the presence of:
- Patches that appear crusty or scaly on the surface.
- These patches often have a yellow or brown hue.
- They are primarily located on the scalp but can extend to other areas.
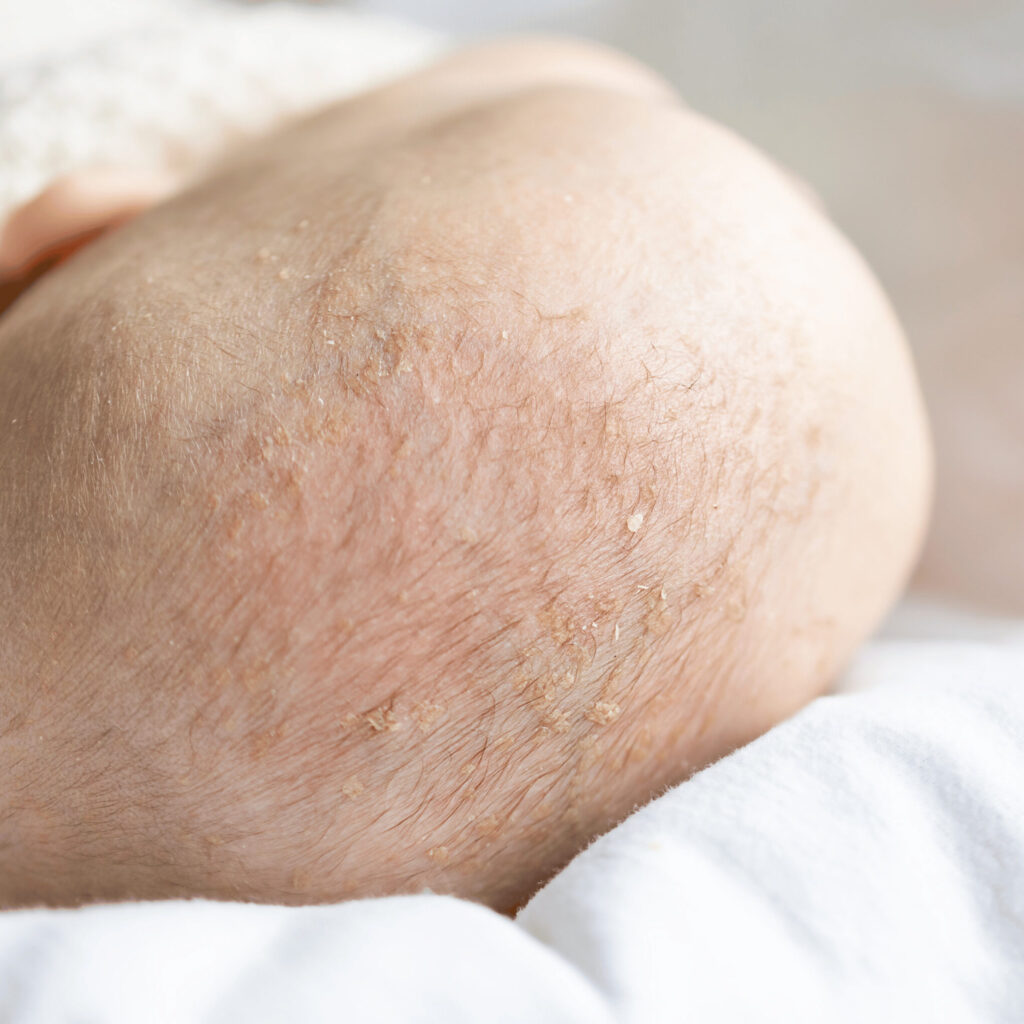
2. Flaky Skin
Similar to dandruff in adults:
- The affected area sheds flaky skin.
- These flakes may be white or yellowish.
- The skin underneath might look red or inflamed.
3. Oily or Greasy Skin
Excess production of sebum can result in:
- Parts of the skin appear shiny or oily.
- This symptom often coexists with the flaky patches, making the area feel greasy to the touch.
4. Mild Redness
Cradle cap may cause:
- The skin beneath the flaky patches turns red.
- This redness is mild and does not indicate a severe skin infection.
It’s essential to note that while these symptoms can be apparent, the cradle cap is generally not associated with pain or discomfort for the baby. However, if any of these symptoms seem severe or spread rapidly, it’s advisable to consult with a pediatrician for a thorough evaluation.
Diagnosis of Cradle Cap
When suspecting cradle cap, or infantile seborrheic dermatitis, obtaining a correct diagnosis is crucial. Here’s how medical professionals typically approach the diagnosis:
1. Physical Examination
The primary method for diagnosing cradle caps is through:
- A thorough visual examination of the affected areas.
- The distinctive appearance of yellow or brown scaly patches, especially on the scalp, often points directly to the cradle cap.
2. Medical History
To ascertain the condition:
- The pediatrician may ask questions about the baby’s health history and any family history of skin conditions.
- Understanding the onset and progression of the symptoms can provide valuable clues.
3. Differentiation from Other Conditions
It’s essential to distinguish cradle caps from other skin disorders. Therefore:
- The doctor may look for signs of other skin conditions such as eczema, psoriasis, or a fungal infection.
- This differentiation ensures that the baby receives appropriate care and that other skin conditions aren’t misdiagnosed as cradle caps.
4. Rarely, Skin Biopsy
In very rare cases, when the diagnosis isn’t clear:
- A small sample of the affected skin might be taken for examination under a microscope.
- This method can help identify or rule out other skin disorders.
For most infants, a straightforward physical examination and discussion of symptoms are sufficient to diagnose cradle cap. However, if there are any doubts or concerns about the diagnosis, parents should always seek a second opinion or further consultation with a dermatologist.
Treatment of Cradle Cap
Addressing cradle cap, or infantile seborrheic dermatitis, involves a combination of home remedies and medical interventions. Here’s a structured approach to its treatment:
1. Gentle Cleaning
Maintaining scalp hygiene is fundamental:
- Wash the baby’s scalp with a mild shampoo regularly.
- Gently massaging the scalp can help in loosening scales and improving blood circulation.
2. Natural Oils
Using natural oils can soften and remove crusty flakes:
- Apply oils like coconut oil, almond oil, or olive oil to the affected area.
- After a few minutes, use a soft brush or cloth to gently remove the loosened scales5.
- Ensure to wash off the oil afterward to prevent further buildup.
3. Medicated Shampoos
In persistent cases:
- Pediatricians may recommend over-the-counter or prescription shampoos formulated for cradle cap6.
- These shampoos often contain ingredients like ketoconazole, selenium sulfide, or salicylic acid.
- It’s vital to follow the doctor’s instructions and ensure that these shampoos do not irritate the baby’s eyes.
4. Topical Creams
For severe or persistent cases:
- A doctor might prescribe topical corticosteroids or antifungal creams.
- These help reduce inflammation and treat any potential fungal overgrowth.
5. Avoid Irritants
To minimize exacerbation:
- Refrain from using products with potential irritants on the baby’s scalp.
- Opt for hypoallergenic or baby-specific products which are milder and gentler.
6. Regular Monitoring
Continual observation is essential:
- Keep track of any changes or spread of the condition.
- If the cradle cap doesn’t improve or worsens, consult a pediatrician.
While cradle cap is often a temporary condition that resolves on its own, effective treatment can alleviate symptoms and enhance the baby’s comfort. Always prioritize safety and consult with healthcare professionals before starting or changing treatments.

Complications of Cradle Cap
While cradle cap, or infantile seborrheic dermatitis, is generally a benign and self-limiting condition, in some rare instances, complications may arise. Awareness of these potential issues ensures timely intervention and care.
1. Infection
The most common complication associated with cradle caps is:
- Secondary bacterial or fungal infections can occur if the skin gets broken or irritated.
- Symptoms include increased redness, warmth, swelling, or oozing from the affected areas.
2. Spread to Other Areas
Though primarily found on the scalp:
- Cradle caps can spread to other parts of the body, such as the eyebrows, eyelids, ears, nose, and groin.
- This spread might necessitate more comprehensive treatment approaches.
3. Persistent Skin Issues
While cradle cap often resolves on its own:
- Some infants may experience prolonged or recurrent bouts.
- Persistent cases may require a more prolonged period of treatment or a different therapeutic approach.
4. Skin Discoloration
Following the resolution of the cradle cap:
- Some babies might have temporary skin discoloration in the affected areas.
- The skin might appear lighter or darker but generally returns to its normal shade over time.
5. Hair Loss
In areas heavily affected by cradle caps:
- Temporary hair loss might occur due to scaling and inflammation.
- The hair typically grows back once the condition is treated and the inflammation subsides.
It’s important to note that while complications can occur, they are not common and are generally manageable with proper care. Parents and caregivers should consult with a pediatrician if they notice any signs of complications or if the condition does not seem to be improving with standard treatments.
Prevention of Cradle Cap
Although cradle cap is a common condition in infants, there are steps that parents and caregivers can take to reduce its likelihood or severity. Implementing preventive measures can assist in keeping the infant’s skin healthy.
1. Regular Cleansing
Routine hygiene can help in preventing sebum buildup:
- Wash the baby’s scalp with a mild baby shampoo regularly.
- Rinse thoroughly to ensure no residue remains.
2. Avoid Overwashing
While cleanliness is essential:
- Overwashing can strip the scalp of natural oils, potentially worsening the condition.
- It’s a balance between maintaining cleanliness and not over-drying the scalp.
3. Gentle Brushing
To remove potential scales:
- Use a soft-bristled brush to gently comb the baby’s scalp7.
- This can help in detaching loose flakes and stimulating the scalp.
4. Moisturize Appropriately
For babies with drier skin:
- A mild, hypoallergenic baby oil or lotion can be beneficial.
- However, avoid excessive use as it can lead to further oil buildup.
5. Be Cautious with Products
Always ensure:
- The use of baby-specific or hypoallergenic products to avoid potential irritants.
- Reading ingredient lists can help identify any components that might be problematic.
6. Regular Check-ups
Routine pediatric visits can:
- Help monitor any early signs of cradle cap.
- Allow for early intervention if needed.
While it may not be possible to entirely prevent cradle caps, adopting these preventive measures can reduce the likelihood or severity of their occurrence. Regular monitoring and early intervention remain essential for ensuring the baby’s skin health and comfort.
Prognosis of Cradle Cap
Cradle cap, known clinically as infantile seborrheic dermatitis, is a common condition affecting many infants. Understanding its prognosis can provide reassurance to concerned parents and caregivers.
1. Self-limiting Nature
One of the defining characteristics of cradle cap is:
- It’s typically a self-limiting condition, meaning it often resolves on its own without the need for medical treatment.
2. Temporary Condition
For most infants:
- Cradle cap is a transient phase, usually presenting within the first few months of life.
- Most cases are resolved by the child’s first birthday, though it can occasionally persist a bit longer.
3. Rare Complications
While generally benign:
- Complications such as secondary bacterial or fungal infections can arise if not properly managed.
- However, with appropriate care, these complications are infrequent and readily treatable.
4. Potential Recurrence
It’s important to note:
- Some children may experience recurrences of seborrheic dermatitis in adolescence or adulthood, though it typically presents differently than cradle cap in infants.
5. Good Overall Outcome
In the grand scheme:
- The vast majority of infants with cradle caps experience no long-term effects on their scalp or skin health.
The prognosis for cradle cap is overwhelmingly positive. Though it can be a source of concern for new parents, with proper care and monitoring, it usually poses little risk and resolves without leaving lasting effects.

Living with Cradle Cap
Living with a cradle cap, while typically a short-lived experience for most infants and their caregivers, requires understanding, care, and patience. Here are some insights into managing daily life with this condition:
1. Daily Care Routine
Establishing a consistent skin-care routine is paramount:
- Gently cleanse the baby’s scalp with a mild shampoo to prevent scale buildup.
- Remember that overbathing can exacerbate the condition, so balance is key.
2. Stay Informed
Knowledge alleviates anxiety:
- Educate yourself about cradle cap, its nature, and the fact that it’s generally not a painful or itchy condition for the baby.
- Understand that its appearance is often more concerning to adults than it is harmful to the infant.
3. Seek Support
You’re not alone in this:
- Connect with other parents or caregivers who have experience with cradle caps.
- Pediatricians, dermatologists, or parent support groups can provide valuable insights and reassurance.
4. Avoid Over-treatment
While it’s natural to want to resolve the condition swiftly:
- Refrain from trying too many treatments simultaneously.
- Over-treatment can irritate the skin further or lead to unnecessary complications.
5. Clothing and Bedding
Comfort is crucial:
- Opt for soft, breathable materials for both clothing and bedding to reduce potential irritation.
- Regularly wash and change bedding to ensure a clean environment.
6. Regular Monitoring
Stay vigilant:
- Monitor the condition and take note of any significant changes or potential complications.
- Keeping a photo diary can help track the progress or recurrence of the condition over time.
7. Monitor and Document
Stay vigilant:
- Keep a close eye on the affected areas and document any significant changes.
- Photos and notes can be useful for tracking progress or when discussing concerns with a pediatrician.
While living with a cradle cap might require some adjustments to daily routines, it’s important to remember that the condition is temporary. With consistent care, understanding, and support, both the baby and caregivers can navigate this phase with minimal disruption and maximum comfort.
When to See Your Pediatrician
While cradle cap is generally a mild condition, there are instances when it’s essential to seek advice or intervention from a pediatrician. Recognizing these signs ensures the infant receives appropriate care in a timely manner.
1. Persistence of Symptoms
While cradle cap often resolves on its own:
- If symptoms persist beyond a few months or don’t show signs of improvement despite home care, it’s prudent to consult a pediatrician.
2. Signs of Infection
Infection can complicate cradle cap:
- If the affected areas become increasingly red, swollen, warm to the touch, or start oozing pus or fluid, it’s time to see the doctor.
- The presence of fever in the baby is also a concerning sign that requires medical attention.
3. Spread Beyond the Scalp
Although cradle cap primarily affects the scalp:
- If the condition spreads to other parts of the body, especially the face or diaper area, a pediatrician’s evaluation can help determine if additional treatment is necessary8.
4. Intense Itching or Discomfort
While some mild itching can be typical:
- If the baby seems excessively bothered, is constantly scratching, or appears restless or agitated due to the affected areas, a visit to the pediatrician is warranted.
5. Skin Discoloration
After the resolution of the scales:
- If the skin remains discolored or you notice any unusual marks or pigmentation, a professional evaluation can provide clarity on the condition.
6. Excessive Hair Loss
While some hair loss can occur:
- If it seems significant or you notice bald patches, it’s good to have a pediatrician evaluate the situation.
7. Baby’s Discomfort
Always prioritize the infant’s well-being:
- If the baby seems particularly uncomfortable, is scratching the affected area often, or is more fussy than usual, these might be indicators to seek expert advice9.
8. Unusual Appearance
Trust your instincts:
- If the patches or scales look different from typical cradle cap descriptions, or if there’s a sudden change in appearance, seek a pediatrician’s advice.
While cradle cap is common and usually harmless, being observant and proactive in seeking medical guidance when necessary ensures the baby’s well-being. It’s always better to err on the side of caution when it comes to the health and comfort of an infant.

Final Thoughts
Cradle cap is a common, typically harmless condition seen in many infants. Though it can concern parents due to its appearance, it’s not a sign of poor hygiene or neglect. Its root causes can range from hormonal shifts to the maturation of the baby’s sebaceous glands.
Remember, every child’s journey is unique. While one infant might experience a brief appearance of a cradle cap, another might have a more prolonged bout. The key lies in consistent care, observation, and seeking guidance when needed. With time, patience, and the right approach, the cradle cap will be a fleeting chapter in the vast narrative of a child’s growth and development.
FAQs
Sources
- Nobles, Timothy, et al. “Cradle Cap.” PubMed, StatPearls Publishing, 2022, www.ncbi.nlm.nih.gov/books/NBK531463/ . Accessed 7 Oct. 2023. ↩︎
- https://www.facebook.com/WebMD. “What Is Cradle Cap?” WebMD, WebMD, Feb. 2017, www.webmd.com/skin-problems-and-treatments/treating-cradle-cap-in-children . Accessed 7 Oct. 2023. ↩︎
- “Cradle Cap.” Raising Children Network, raisingchildren.net.au/newborns/health-daily-care/health-concerns/cradle-cap . Accessed 7 Oct. 2023. ↩︎
- “Cradle Cap: What It Is, Symptoms & Treatment.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/15786-cradle-cap-seborrheic-dermatitis-in-infants . Accessed 7 Oct. 2023. ↩︎
- “Cradle Cap (Seborrheic Dermatitis) in Infants (for Parents) – KidsHealth.” Kidshealth.org, 2019, kidshealth.org/en/parents/cradle-cap.html . Accessed 7 Oct. 2023. ↩︎
- “How to Treat Cradle Cap.” Www.aad.org, www.aad.org/public/everyday-care/hair-scalp-care/scalp/treat-cradle-cap . Accessed 7 Oct. 2023. ↩︎
- “Cradle Cap.” Nhs.uk, 24 Oct. 2017, www.nhs.uk/conditions/cradle-cap/ . Accessed 7 Oct. 2023. ↩︎
- “Cradle Cap – Symptoms and Causes.” Mayo Clinic, www.mayoclinic.org/diseases-conditions/cradle-cap/symptoms-causes/syc-20350396 . Accessed 7 Oct. 2023. ↩︎
- “Cradle Cap.” HealthyChildren.org, www.healthychildren.org/English/ages-stages/baby/bathing-skin-care/Pages/Cradle-Cap.aspx . Accessed 7 Oct. 2023. ↩︎