Random muscle spasms or an unexpected bout of dizziness can often be brushed off as just ‘one of those days’. But what if there’s more to it?
It’s time to know more about Multiple Sclerosis. Curious about the details? Read on.
- What is Multiple Sclerosis?
- Types of Multiple Sclerosis (MS)
- Symptoms of Multiple Sclerosis (MS)
- Causes of Multiple Sclerosis (MS)
- Risk Factors for Multiple Sclerosis (MS)
- Triggers of Multiple Sclerosis (MS) Flare-ups
- Diagnosis of Multiple Sclerosis (MS)
- Treatment of Multiple Sclerosis (MS)
- Complications of Multiple Sclerosis (MS)
- Prevention in Multiple Sclerosis (MS)
- Final Thoughts
- FAQs
What is Multiple Sclerosis?
Multiple Sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system, specifically the brain and spinal cord1. In MS, the immune system mistakenly attacks the protective covering of nerve fibers, known as myelin, leading to inflammation and damage.
This damage disrupts the normal flow of electrical impulses along the nerves, resulting in various neurological symptoms. According to WHO, it is estimated that over 1.8 million people have Multiple Sclerosis worldwide2.
Types of Multiple Sclerosis (MS)
Multiple Sclerosis (MS) manifests in distinct forms, each with its own pattern of symptoms and progression. Recognizing these types is crucial for diagnosis, treatment, and prognosis.
Relapsing-Remitting MS (RRMS)
RRMS is marked by clear episodes of increased disease activity or relapses, followed by periods of remission where the person may partially or fully recover.
This form is the most common, with about 85% of MS patients initially diagnosed with RRMS.
Secondary Progressive MS (SPMS)
A stage that follows RRMS. With SPMS, there’s a steady progression of symptoms. Relapses can still occur but are less frequent.
Most individuals with RRMS will transition to SPMS, typically after 10-20 years.
Primary Progressive MS (PPMS)
From the onset, PPMS sees a continuous worsening of symptoms without distinct relapses or remissions. PPMS is less common, affecting roughly 10-15% of MS patients.
Clinically Isolated Syndrome (CIS)
A single, first episode of neurological symptoms due to demyelination. It lasts at least 24 hours. While not always followed by further symptoms, it may be a precursor to MS.
An estimated 30-70% of individuals with CIS will develop MS within several years.
Symptoms of Multiple Sclerosis (MS)
Multiple Sclerosis (MS) targets the central nervous system, producing a variety of symptoms that can fluctuate in severity based on individual cases and disease progression.
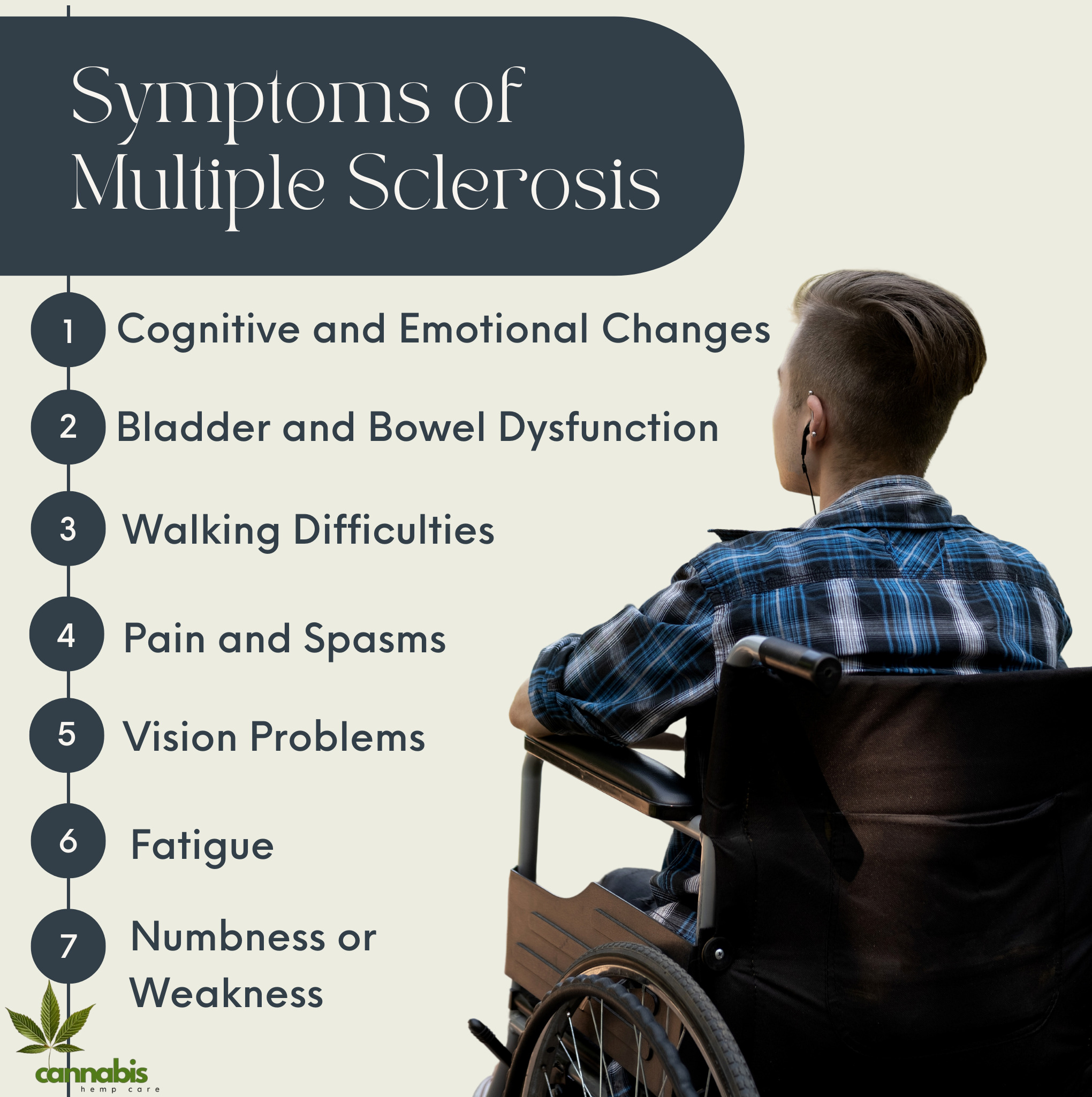
Fatigue
Overwhelming tiredness, often severe enough to disrupt daily activities, is a common complaint among Multiple Sclerosis patients.
Numbness or Weakness
Typically, this impacts one side of the body, often initiating in the legs. It arises from damaged nerve fibers interrupting electrical impulses.
Vision Problems
Inflammation of the optic nerve can lead to blurred or double vision and sometimes results in partial or complete vision loss3.
Pain and Spasms
Chronic pain, notably in the back or legs, is frequent. Muscle spasms, especially in the legs, are also a common symptom.
Walking Difficulties
Multiple Sclerosis can result in challenges with walking due to muscle weakness, balance issues, spasticity, or fatigue.
Cognitive and Emotional Changes
Memory issues, mood fluctuations, depression, or other cognitive shifts can be present in some MS patients.
Bladder and Bowel Dysfunction
Symptoms may encompass frequent urination, bladder urgency, or constipation due to the brain’s disrupted signaling with these systems.
It’s essential to note that while these symptoms can be burdensome, understanding them is crucial for effective management and seeking appropriate medical attention.
Causes of Multiple Sclerosis (MS)
Multiple Sclerosis (MS) is a complex disease, and its exact cause remains not fully understood. However, current research points to a combination of genetic, environmental, and possibly viral factors contributing to its development.
Immune System Dysfunction
In MS, the immune system mistakenly targets and damages the myelin sheath4, the protective layer around nerve fibers in the central nervous system. The reason for this aberrant immune response is not fully understood.
Genetic Factors
While Multiple Sclerosis isn’t directly inherited, having a family member with MS might increase an individual’s risk. Specific genes appear to increase susceptibility.
Environmental Factors
Several studies indicate that various environmental factors might increase the risk of developing MS. For instance:
- Vitamin D: Low levels of vitamin D, potentially due to less sunlight exposure, have been linked with a higher risk of MS.
- Infections: Some viruses, like the Epstein-Barr virus, have been suggested as potential triggers for MS, though the evidence isn’t conclusive.
Other Risk Factors
Additional factors that may influence the risk of Multiple Sclerosis include age, gender, and certain infections. However, their precise role in causing MS remains a subject of research.
While the exact causes of Multiple Sclerosis are still being unraveled, a blend of genetic predisposition and environmental triggers seems to play a role. Further research is ongoing to pinpoint the specific factors leading to the development of MS.

Risk Factors for Multiple Sclerosis (MS)
The development of Multiple Sclerosis (MS) is influenced by several risk factors. While these don’t directly cause the disease, they may increase an individual’s likelihood of developing it.
Age
Multiple Sclerosis is most commonly diagnosed in people aged 20 to 405, although it can develop at any age.
Gender
Women are about 2-3 times more likely than men to develop RRMS, the most common form of MS6.
Genetic Background
Having a family member, especially a sibling, with Multiple Sclerosis increases one’s risk, pointing to a genetic predisposition.
Geographical Location
Multiple Sclerosis prevalence increases the farther one is from the equator, suggesting a possible environmental link, potentially related to sunlight exposure and vitamin D levels.
Infection History
Certain infections, notably Epstein-Barr virus, have been associated with a higher risk of MS.
Other Autoimmune Diseases
Individuals with autoimmune conditions like type 1 diabetes, thyroid disease, or inflammatory bowel disease might have a slightly increased risk of developing MS.
Smoking
Smokers have a higher risk of contracting Multiple Sclerosis compared to non-smokers, and smoking can also accelerate disease progression.
In understanding these risk factors, individuals can make informed decisions about their health and be vigilant about potential MS symptoms. Awareness aids in early diagnosis and management.
Triggers of Multiple Sclerosis (MS) Flare-ups
For people with Multiple Sclerosis (MS), certain factors can trigger or exacerbate symptoms, leading to relapses or flares. It’s essential to identify these triggers to effectively manage and potentially reduce the occurrence of flares.
Stress
Emotional or physical stress can precipitate or amplify MS symptoms. Managing stress through relaxation techniques or therapy can be beneficial.
Infections
Bacterial or viral infections can lead to Multiple Sclerosis relapses. Common culprits include urinary tract infections or viral illnesses like the flu.
Temperature Increases
Heat, including elevated body temperature, hot baths, or exposure to direct sunlight, can worsen symptoms temporarily for some Multiple Sclerosis patients.
Physical Exertion
Overexertion or fatigue can trigger symptoms or make existing ones more pronounced.
Certain Medications
Some drugs can exacerbate MS symptoms. It’s vital for patients to discuss potential risks with healthcare professionals before starting new medications.
Vaccinations
While most vaccines are safe for Multiple Sclerosis patients, some can lead to flare-ups. It’s essential to consult with a medical professional before receiving vaccinations.
Being aware of these triggers allows those with MS to take preventative measures, ensuring more effective disease management and symptom control.
Diagnosis of Multiple Sclerosis (MS)
Diagnosing Multiple Sclerosis (MS) involves a combination of clinical evaluations, imaging studies, and other tests. Since Multiple Sclerosis symptoms can mirror other medical conditions, a comprehensive approach ensures accurate diagnosis.
Medical History
A detailed account of symptoms, their progression, and any family history of neurological disorders can provide valuable insights.
Neurological Examination
Doctors assess movement, balance, speech, and other functions to identify signs of neurological abnormalities.
Magnetic Resonance Imaging (MRI)
An MRI can show areas of MS-related damage in the brain and spinal cord. It’s a crucial tool in both diagnosis and monitoring disease progression.
Spinal Fluid Analysis
A lumbar puncture or spinal tap can obtain cerebrospinal fluid7. The presence of certain proteins can indicate inflammation and potential Multiple Sclerosis activity.
Evoked Potentials
These tests measure electrical activity in the brain in response to stimuli. Delays in response time can suggest damage to the pathways that conduct sensory information.
Blood Tests
While no blood test can diagnose Multiple Sclerosis alone, blood tests help rule out other conditions with similar symptoms.
A definitive MS diagnosis often requires evidence of damage in at least two separate areas of the central nervous system, occurring at different times. Regular reviews and monitoring are essential, as the disease’s nature and symptoms can evolve over time.
Treatment of Multiple Sclerosis (MS)
Treatment for Multiple Sclerosis (MS) focuses on managing symptoms, reducing the frequency of relapses, and slowing disease progression. There’s no cure for MS, but various treatments can improve patients’ quality of life.
Disease-Modifying Therapies (DMTs)
These drugs, often taken long-term, aim to reduce the rate and severity of relapses and slow the progression of MS. Examples include interferons, glatiramer acetate, and oral medications like dimethyl fumarate.
Corticosteroids
Used to reduce nerve inflammation during a relapse, these drugs can shorten the duration and intensity of flare-ups8.
Symptomatic Treatments
Depending on the symptom, various medications can be prescribed:
- Muscle spasticity: Baclofen or tizanidine
- Fatigue: Modafinil or amantadine
- Neuropathic pain: Gabapentin or pregabalin
Physical Therapy
Tailored exercise programs can help manage symptoms like muscle stiffness, balance issues, and fatigue.
Plasma Exchange (Plasmapheresis)
For severe relapses unresponsive to steroids, this procedure involves removing and treating the patient’s blood before returning it to the body, removing harmful antibodies in the process.
Lifestyle and Wellness
Maintaining a balanced diet, engaging in regular exercise, and avoiding triggers like excessive heat can play a role in managing MS symptoms.
Early and ongoing treatment, combined with regular monitoring, can help those with MS lead full, active lives despite the challenges of the disease.
Complications of Multiple Sclerosis (MS)
Multiple Sclerosis (MS) can lead to several complications over time. These complications can arise directly from the disease or result from its various symptoms.
Physical Challenges
- Mobility issues: Many with MS face difficulty walking, often requiring assistive devices.
- Muscle spasms and stiffness: Prolonged muscle issues can cause discomfort and restrict movement.
- Coordination and balance problems: These can increase the risk of falls or injuries.
Neurological Complications
- Paralysis: In advanced cases, patients may experience paralysis, typically in the legs.
- Tremors: Involuntary shaking can affect the hands or other parts of the body.
- Epilepsy: Some MS patients develop seizures.
Bladder and Bowel Issues
- Urinary complications: Include urgency, frequency, and retention.
- Bowel problems: Constipation is common, as is loss of bowel control in severe cases.
Mental Health Concerns
- Depression: A significant proportion of Multiple Sclerosis patients experience depression.
- Cognitive changes: Some individuals face issues with memory, attention, or problem-solving.
Sexual Dysfunction
Both men and women with Multiple Sclerosis might experience reduced sexual desire, sensation, or responsiveness.
Vision Problems
Prolonged inflammation of the optic nerve can lead to partial or complete vision loss.
In the context of these complications, regular medical monitoring is essential. With timely intervention, many complications can be managed or mitigated, ensuring a better quality of life for those with MS.
Prevention in Multiple Sclerosis (MS)
Currently, there is no known method to prevent the onset of Multiple Sclerosis (MS) due to its unclear and multifaceted causes. However, measures can be taken to possibly reduce the risk or prevent the exacerbation of symptoms once diagnosed.
Vitamin D
There’s evidence suggesting a potential link between low levels of vitamin D and the onset or severity of MS. Regular sun exposure and vitamin D supplementation might reduce the risk.
No Smoking
Smoking has been identified as a risk factor for developing MS and accelerating its progression. Quitting smoking is advisable.
Healthy Lifestyle
Maintaining a balanced diet, regular exercise, and managing stress might play a role in reducing the risk or severity of MS symptoms.
Regular Medical Check-ups
Frequent health screenings can help detect and address potential risk factors, thereby reducing the chances of developing associated conditions or complications.
Avoid Infections
As some infections are thought to trigger MS or its flare-ups, it’s beneficial to practice good hygiene, stay updated on vaccinations, and seek prompt medical attention when ill.
While it’s impossible to guarantee the prevention of MS, understanding potential risk factors and adopting a proactive approach to health can help in managing the disease and ensuring a better quality of life.

Final Thoughts
Understanding Multiple Sclerosis is the first step toward managing and living with it. With the right information and support, individuals with MS can navigate the challenges and lead fulfilling lives.
Staying informed and proactive is key. Knowledge isn’t just power; it’s empowerment.
FAQs
Sources
- —. “Multiple Sclerosis.” Cleveland Clinic, 10 Feb. 2021, my.clevelandclinic.org/health/diseases/17248-multiple-sclerosis . Accessed 7 Oct. 2023. ↩︎
- “Multiple Sclerosis.” Www.who.int, www.who.int/news-room/fact-sheets/detail/multiple-sclerosis Accessed 7 Oct. 2023. ↩︎
- “Multiple Sclerosis (MS).” Www.hopkinsmedicine.org, www.hopkinsmedicine.org/health/conditions-and-diseases/multiple-sclerosis-ms#:~:text=Multiple%20sclerosis%20(MS)%20is%20a%20chronic%20disease%20of%20the%20central. Accessed 7 Oct. 2023. ↩︎
- Medline Plus. “Multiple Sclerosis: MedlinePlus Medical Encyclopedia.” Medlineplus.gov, 2016, medlineplus.gov/ency/article/000737.htm . Accessed 7 Oct. 2023. ↩︎
- https://www.facebook.com/WebMD. “What Is Multiple Sclerosis?” WebMD, WebMD, 31 Dec. 2002, www.webmd.com/multiple-sclerosis/what-is-multiple-sclerosis . Accessed 7 Oct. 2023. ↩︎
- —. “Multiple Sclerosis – Symptoms and Causes.” Mayo Clinic, 24 Dec. 2022, www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269 . Accessed 7 Oct. 2023. ↩︎
- National Institute of Neurological Disorders and Stroke. “Multiple Sclerosis | National Institute of Neurological Disorders and Stroke.” Www.ninds.nih.gov, 2023, www.ninds.nih.gov/health-information/disorders/multiple-sclerosis . Accessed 7 Oct. 2023. ↩︎
- —. “Multiple Sclerosis.” NHS, NHS, 22 Mar. 2022, www.nhs.uk/conditions/multiple-sclerosis/ . Accessed 7 Oct. 2023. ↩︎