Imagine you wake up one morning to find unfamiliar red patches on your skin, feeling a mix of confusion and concern. You’re not alone. Many across the globe face this very situation when encountering their first bout with psoriasis.
But what is psoriasis exactly? What causes it, and how can it be managed? Curious? Let’s unravel the mystery together.
What is Psoriasis?
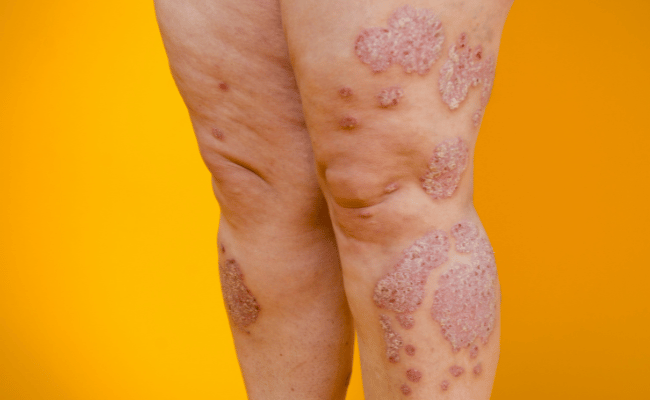
Psoriasis is a chronic disease where the immune system mistakenly attacks healthy skin cells, causing a rapid buildup on the skin’s surface. The excess skin cells form red patches and scales, which may be itchy and painful. It’s a persistent disease with symptoms fluctuating from mild to severe over time.
Who Gets Psoriasis?
Psoriasis can affect anyone, regardless of age, but it’s more commonly diagnosed in adults. Both men and women are equally affected1.
Types of Psoriasis and Affected Parts
Psoriasis is a multifaceted skin condition, that displays itself in various forms. While the underlying immune dysfunction is common to all, the presentation on the skin can greatly differ. It’s essential to recognize and differentiate these types, as the management and implications can vary.
| Types of Psoriasis | Description | Appearance | Common Affected Parts |
| Plaque Psoriasis (Psoriasis Vulgaris) | This is the most prevalent form of psoriasis, accounting for about 80-90% of cases2. | Raised, red, inflamed patches covered with | Elbows, knees, scalp, lower back |
| Guttate Psoriasis | Often found in children and young adults, this type is usually triggered by bacterial infections, notably strep throat. | Small, dot-like lesions. | Torso, arms, legs |
| Pustular Psoriasis | Uncommon, these pustules contain white blood cells and are not an infection nor contagious. | White pustules surrounded by red skin. | Hands, feet |
| Inverse Psoriasis (Flexural Psoriasis) | Often found in skin folds. It’s more common in overweight individuals and is worsened by friction and sweating. | Smooth, red patches of skin, inflamed, may appear shiny. | Armpits, groin, under the breasts, other skin folds. |
| Erythrodermic Psoriasis | Armpits, groin, under the breasts, and other skin folds. | Widespread redness covering large areas of the body, severe itching, and pain. | Nearly the entire skin surface |
Identifying the type of psoriasis is fundamental to tailoring an effective treatment strategy, ensuring both the mitigation of symptoms and the enhancement of the patient’s quality of life. Always consult with a dermatologist or healthcare provider for an accurate dia

Symptoms
Psoriasis is characterized by a range of symptoms, varying with its type and severity.
Common Symptoms
- Red, Raised Patches: These inflamed patches, often covered with silvery scales, are most commonly associated with plaque psoriasis.
- Small, Scaly Spots: Typically seen in children and young adults, these are characteristic of guttate psoriasis.
- Dry Skin: The skin may crack and bleed in certain areas.
- Itching or Burning Sensation: Many individuals with psoriasis report persistent itching or a burning sensation in the affected areas.
- Thick, Pitted Nails: Psoriasis can affect fingernails and toenails, leading to abnormal nail growth, discoloration, and pitting.
- Painful, Swollen Joints: This symptom is often indicative of psoriatic arthritis, a related condition.
Specific to Certain Types
- Pus-filled Blisters: Seen in pustular psoriasis, these blisters are non-infectious.
- Smooth Patches in Skin Folds: This red, inflamed skin without scales is associated with inverse psoriasis.
- Widespread Redness with Severe Itching: A sign of erythrodermic psoriasis, this can be especially intense and cover large areas of the body.
Associated Symptoms
Certain individuals may also experience related symptoms, such as:
- Eye Conditions: Including conjunctivitis, uveitis, and blepharitis.
- Emotional Impact: Due to the visible nature of the condition, some people might experience feelings of low self-esteem, embarrassment, or depression.
While these symptoms provide a comprehensive guide to recognizing psoriasis, individual experiences may vary. If you or someone you know presents these signs, consulting a dermatologist for a definitive diagnosis is crucial.
When to see your doctor
Identifying the signs of psoriasis is crucial, but knowing when to seek medical intervention is equally important.
Primary Indications
Persistent Red Patches
If you notice red patches of skin that are covered in silvery scales and these patches persist or worsen over time, it’s essential to consult a doctor.
Severe Itching, Burning, or Soreness
Discomfort that impedes daily activities or disrupts sleep should be taken seriously.
Joint Discomfort
Swelling, stiffness, or pain in the joints can be indicative of psoriatic arthritis, a related condition, and should prompt a medical consultation.
Worsening or Spreading Symptoms
Rapid Progression
If an initial small patch or rash begins to spread rapidly, it’s imperative to seek medical advice.
Appearance of Pustules
Pus-filled blisters or bumps, especially if they’re accompanied by fever or muscle weakness, need immediate medical attention.
After Starting New Medications
If you observe psoriasis symptoms shortly after starting a new medication, it’s crucial to inform your doctor, as some medications can trigger or exacerbate psoriasis.
Emotional or Psychological Distress
The physical manifestations of psoriasis can sometimes lead to anxiety, depression, or other psychological challenges. If you feel emotionally overwhelmed, it’s essential to discuss these feelings with a healthcare professional.
Recognizing the signs of psoriasis early and seeking timely medical intervention can mitigate the disease’s progression and enhance the quality of life.

Causes
Understanding the underlying causes of psoriasis helps in better management and treatment of the condition. It’s known to be an immune-mediated disorder with a complex interplay of genetic and environmental factors.
Genetic Factors
- Genetic Predisposition: Psoriasis tends to run in families, suggesting a genetic link. Studies have identified specific genes associated with a higher risk of developing the condition. For instance, having a parent with psoriasis increases an individual’s risk by about 10%, and if both parents are affected, the risk can rise to 50%.
Immune System
- T cells Activation: T cells, a type of T cell, become overactive in psoriasis sufferers. These activated T cells lead to an increased production of healthy skin cells, T cells, and white blood cells, causing the characteristic scales of psoriasis3.
Environmental Triggers
- Infections: Streptococcal throat infections can trigger the onset of guttate psoriasis or exacerbate existing conditions.
- Injury: A phenomenon called the Koebner response can occur, where new psoriasis patches develop at sites of skin injury, such as cuts, burns, or insect bites.
- Stress: High-stress levels can initiate or amplify the symptoms.
- Medications: Certain medications, including specific antihypertensives, antimalarials, and lithium, can either induce psoriasis or exacerbate it.
- Other factors: Obesity, smoking, and alcohol consumption have also been linked to the onset or exacerbation of psoriasis4.
While the exact cause of psoriasis remains elusive, a combination of genetic predisposition, immune system dysfunction, and environmental triggers seem to play significant roles. It’s essential for those with psoriasis or at risk of developing it to be aware of these factors and work towards managing or mitigating them where possible.
Is psoriasis contagious? No, psoriasis is not contagious. You cannot catch it from touching someone who has it, nor can you spread it to other parts of your body through touch.
Diagnosis
Introduction
The diagnosis of psoriasis is primarily clinical, meaning that it is based on a thorough examination of the skin, scalp, and nails by a healthcare professional. However, in some cases, further tests may be needed to confirm the diagnosis and rule out other skin conditions.
Clinical Examination
The primary step in diagnosing psoriasis is a thorough physical examination. A dermatologist will inspect the skin, scalp, nails, and any other affected areas to identify characteristic signs of the condition.
Medical History
A detailed medical history often aids the diagnostic process. The physician will ask about the onset, duration, and progression of symptoms, any previous treatments, and their outcomes. Family history can also play a role since psoriasis has a genetic component.
Biopsy
In cases where the diagnosis isn’t clear-cut, a skin biopsy might be performed. This involves removing a small sample of the affected skin to examine under a microscope. This can confirm the presence of psoriatic skin cells and rule out other skin disorders.
Blood Tests
While there’s no specific blood test for psoriasis, some tests can exclude other conditions with similar symptoms, like rheumatoid arthritis or lupus.
Joint Imaging
For individuals showing signs of psoriatic arthritis, imaging tests like X-rays or MRI might be necessary. These can identify joint damage typical of psoriatic arthritis.
According to the World Health Organization, around 2% to 3% of the global population is affected by psoriasis. Early diagnosis can lead to better management and improved quality of life for these individuals.
Triggers
While the underlying causes of psoriasis stem from genetic and immune system factors, certain triggers can provoke or exacerbate its outbreaks. Recognizing and managing these triggers is pivotal for those looking to control their psoriatic symptoms.
Infections
Specific infections, particularly streptococcal throat infections, can lead to the onset or worsening of psoriasis symptoms, mainly in the case of guttate psoriasis. HIV infection is another potential trigger, often causing more severe symptoms.
Medications
Certain drugs can prompt or intensify psoriasis outbreaks. These include, but are not limited to, lithium (used for bipolar disorder), antimalarial medications, specific beta-blockers (for hypertension), and indomethacin (an anti-inflammatory drug).
Trauma to the Skin
Physical trauma, including cuts, burns, and insect bites, can lead to a new psoriatic lesion on the injured skin. This phenomenon is referred to as the Koebner response.
Stress
Emotional stress is a well-documented trigger for psoriasis. Stress can both instigate new outbreaks and exacerbate existing ones. Managing stress through relaxation techniques or therapy can be beneficial.
Alcohol and Tobacco
Excessive alcohol consumption can potentially trigger psoriasis outbreaks or worsen symptoms. Additionally, tobacco use, especially smoking, increases the risk of developing psoriasis and can also exacerbate the condition.
Hormonal Changes
Fluctuations in hormone levels, such as during puberty, menopause, or pregnancy, can influence psoriasis symptoms.
It’s estimated that up to 90% of psoriasis patients experience exacerbations due to specific triggers. Proper management and awareness of these triggers can significantly improve symptom control and quality of life.
Food Triggers
Diet plays a pivotal role in overall health, and for individuals with psoriasis, specific foods can exacerbate their condition. While responses to food can vary from person to person, certain dietary elements are commonly linked to psoriasis flare-ups.
Alcohol
Regular alcohol consumption can increase the risk of flare-ups. Alcohol can interfere with the effectiveness of psoriasis treatments and is known to trigger outbreaks.
Red Meat and Dairy
Red meat, particularly beef, and dairy products contain a polyunsaturated fat called arachidonic acid. Excess consumption can exacerbate psoriasis symptoms due to the inflammatory nature of this fat.
Processed Foods
Processed foods high in refined sugars, artificial flavors, and preservatives might increase inflammation, aggravating psoriasis.
Nightshades
Vegetables like tomatoes, potatoes, peppers, and eggplants belong to the nightshade family. Some individuals with psoriasis have reported flare-ups after consuming these.
Gluten
For those with a gluten sensitivity or celiac disease, consuming gluten can trigger psoriasis symptoms. Studies have suggested a potential link between psoriasis and celiac disease.
According to a study published in the Journal of the Academy of Nutrition and Dietetics, nearly 25% of individuals with psoriasis reported a sensitivity to gluten, suggesting dietary interventions might benefit some psoriasis patients. Source: Journal of the Academy of Nutrition and Dietetics
Foods That Help Manage
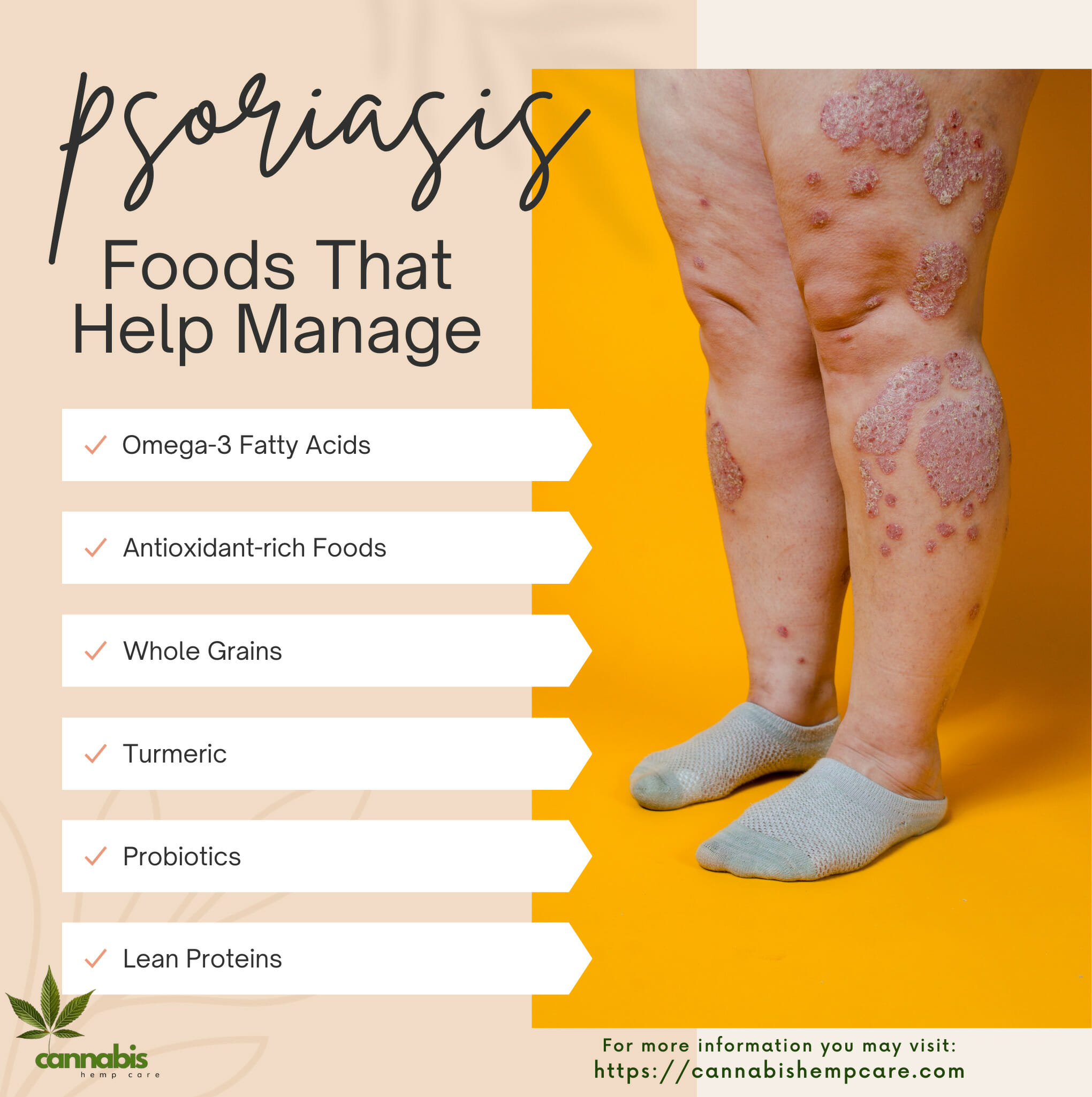
Managing psoriasis often extends beyond topical treatments and medications. Nutrition plays a significant role, with some foods known to alleviate symptoms or reduce flare-ups. Here’s a breakdown of foods that can be beneficial for individuals with psoriasis.
Omega-3 Fatty Acids
Foods rich in omega-3 fatty acids, such as salmon, mackerel, sardines, and flaxseeds, can help reduce inflammation and potentially lessen psoriasis symptoms.
Antioxidant-rich Foods
Fruits and vegetables like blueberries, spinach, cherries, and kale are packed with antioxidants that can combat inflammation and support skin health.
Whole Grains
Whole grains, including quinoa, brown rice, and oats, can support a healthy inflammatory response, potentially benefiting those with psoriasis.
Turmeric
Turmeric contains curcumin, which has powerful anti-inflammatory properties. Incorporating turmeric into the diet or taking supplements may aid in managing psoriasis symptoms.
Probiotics
Probiotics found in yogurt, kefir, and fermented foods can aid in gut health. A balanced gut can impact skin health, potentially reducing psoriasis flare-ups.
Lean Proteins
Lean proteins such as poultry, tofu, and beans can be part of an anti-inflammatory diet, supporting skin health and potentially reducing the severity of psoriasis symptoms.
A study suggested that curcumin might inhibit the inflammatory enzymes associated with psoriasis, indicating its potential therapeutic role.
Risk Factors
Psoriasis, though primarily genetic in nature, can be influenced by various risk factors that either trigger its onset or exacerbate its symptoms. Understanding these factors is essential in managing the condition effectively.
Genetics
A family history of psoriasis can increase one’s risk5. If one parent has psoriasis, there’s an increased likelihood for their child to develop it, and the risk multiplies if both parents have the condition.
Studies have shown that an individual with one parent affected by psoriasis has about a 10% risk of developing the disease, and this risk rises to 50% if both parents have psoriasis6.
Stress
Stress, both emotional and physical, can act as a trigger. Increased stress levels can not only lead to the onset of the disease in susceptible individuals but can also exacerbate existing conditions.
Infections
Certain infections, especially streptococcal infections (like strep throat), can act as triggers for psoriasis in some people, especially children.
Injury to the Skin
Trauma to the skin such as cuts, burns, or insect bites can trigger a phenomenon called the Koebner response, leading to new psoriatic lesions at the site of injury.
Medications
Some medications, like beta-blockers, lithium, and antimalarial drugs, can either induce or exacerbate psoriasis. It’s estimated that drug-induced psoriasis cases account for 2-5% of all psoriasis cases in adults.
Hormonal Changes
Shifts in hormone levels, such as during puberty, menopause, or pregnancy, can influence psoriasis symptoms.
Lifestyle Factors
Excessive alcohol consumption and smoking can exacerbate psoriasis and may diminish the efficacy of treatments.
Obesity
Excess body weight, particularly visceral fat, can lead to increased inflammation in the body, which may worsen psoriasis symptoms. There’s also an observed increased prevalence of psoriasis in individuals with a higher body mass index (BMI). Research indicates that people with a BMI over 30 are twice as likely to have psoriasis compared to those with a lower BMI.

Management and Treatment
Effectively managing psoriasis involves a combination of medical treatments, lifestyle modifications, and addressing any concurrent health issues. Through a collaborative effort between patients and healthcare professionals, it’s possible to control symptoms and improve the quality of life for individuals with psoriasis.
Topical Treatments
The first line of treatment for many psoriasis patients involves the use of topical agents applied directly to the skin.
- Corticosteroids: These are anti-inflammatory creams or ointments that help reduce inflammation and redness.
- Vitamin D analogs: Such as calcipotriene, help slow down the growth of skin cells.
- Coal tar: This is a traditional treatment that can reduce scaling, itching, and inflammation.
About 80% of people with mild to moderate psoriasis can be effectively treated with topical agents alone.
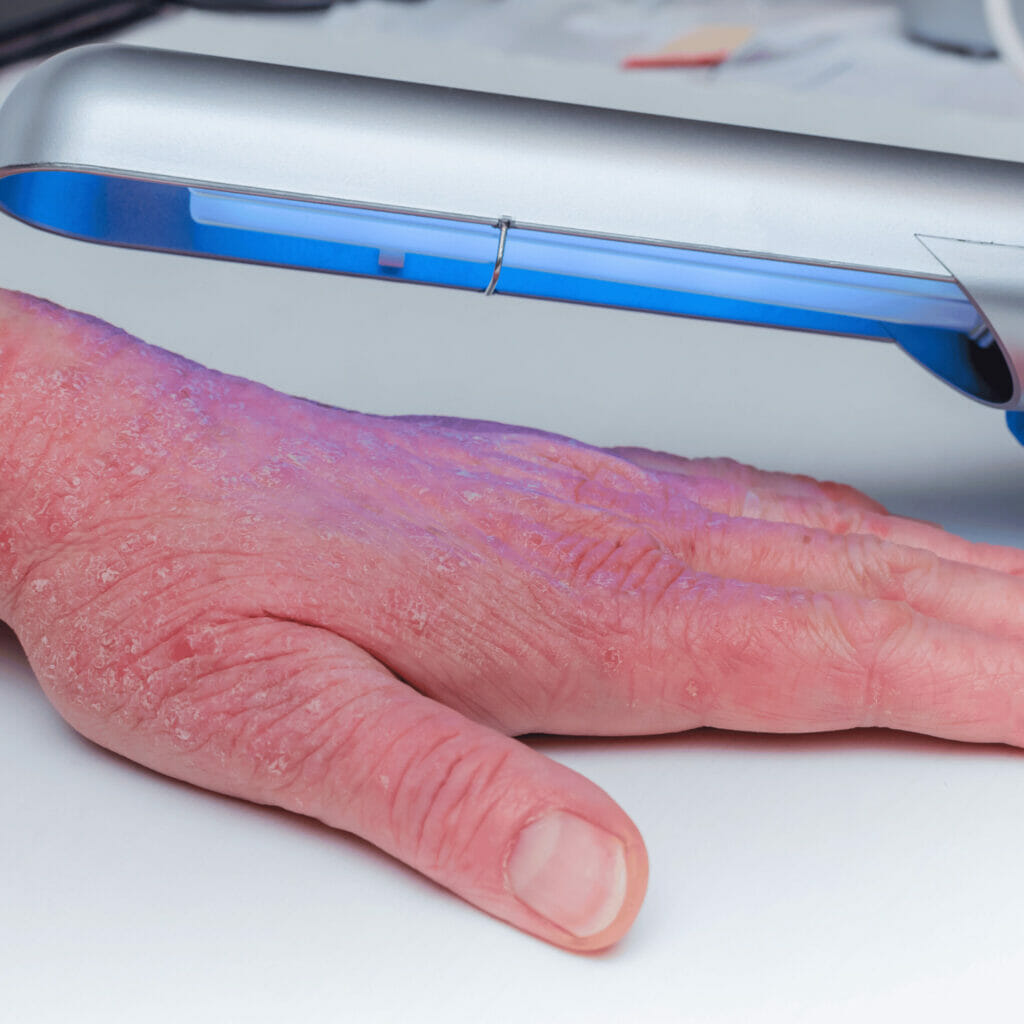
Light Therapy (Phototherapy)
This involves exposing the skin to ultraviolet light under the supervision of a dermatologist. It can be effective for those who don’t respond well to topical treatments. Types include:
- Narrowband UVB therapy: The most common form of light therapy for psoriasis.
- PUVA (psoralen plus ultraviolet A): Combines UVA light with a drug called psoralen.
Systemic Treatments
For moderate to severe psoriasis, or when the disease is more widespread, oral or injected medications may be prescribed.
- Methotrexate: Slows the growth of skin cells and suppresses inflammation.
- Cyclosporine: Suppresses the immune system to halt the rapid turnover of skin cells.
- Retinoids: Derivatives of Vitamin A used to normalize DNA activity in skin cells7.
Alternative Therapies
While not primary treatments, some people find relief with therapies like:
- Aloe Vera: Applied topically can soothe skin and reduce redness and scaling.
- Oregon grape (Mahonia aquifolium): Used in some over-the-counter treatments.
Lifestyle Modifications
A healthy lifestyle can have a profound impact on the management of psoriasis.
- Diet: Consuming a balanced diet with plenty of fruits, vegetables, and whole grains can help reduce inflammation.
- Weight management: Studies suggest a correlation between weight loss and a decrease in the severity of psoriasis symptoms.
In a study, individuals with psoriasis who reduced their weight by just 5% saw significant improvements in their symptoms.
Stress Reduction
Given that stress can be a trigger, strategies such as meditation, deep breathing exercises, and regular physical activity can help manage psoriasis.
Regular Monitoring
Routine check-ups with a dermatologist help in adjusting treatment plans as necessary and monitoring for potential complications, such as psoriatic arthritis.
Support and Education
Joining support groups and getting educated about the condition can help patients cope better. It can also help combat the social isolation that some individuals may feel due to their condition.
45% of psoriasis patients reported that they felt more empowered and better equipped to manage their disease after attending support group sessions.

Prevention
While the onset of psoriasis cannot be completely prevented due to its genetic component, certain measures can be taken to manage potential triggers and reduce the severity or frequency of flare-ups.
Maintain Skin Health
Regular moisturizing can prevent dry skin and reduce the severity of psoriasis symptoms.
- Moisturizing creams: Applying thick ointments like petroleum jelly can lock in moisture and prevent skin dryness. Moisturizing can reduce itchiness by up to 80%.
- Bathing: Using lukewarm water and mild soap can prevent skin irritation.
Limit Alcohol Intake
Excessive alcohol consumption may increase the risk of psoriasis flare-ups and reduce the effectiveness of treatments.
Reduce Stress
Stress is a common trigger for many psoriasis patients.
- Relaxation techniques: Practices like meditation, deep-breathing exercises, and yoga can reduce stress and potentially decrease flare-ups.
Avoid Skin Injuries
Physical trauma can trigger a psoriasis condition known as the Koebner phenomenon.
- Protection: Be cautious during physical activities and protect the skin from cuts, scrapes, and severe sunburn.
Healthy Lifestyle Choices
Adopting a balanced diet and regular exercise routine can potentially help reduce the severity of symptoms.
- Weight management: Obesity is a risk factor for psoriasis. Maintaining a healthy weight might reduce the risk and severity of psoriasis.
Avoid Smoking
Smoking can increase the risk of developing psoriasis and make the disease more severe.
Regular Check-ups
Routine medical check-ups can help monitor health conditions that might contribute to psoriasis or interfere with its treatment.
Complications
Psoriatic Arthritis
One of the most common complications of psoriasis is psoriatic arthritis, an inflammatory joint condition8.
- Symptoms: Joint pain, swelling, and stiffness.
- Affected areas: Typically affects the fingers, toes, spine, and the joints in the hands and feet.
Up to 30% of people with psoriasis will develop psoriatic arthritis.
Cardiovascular Problems
Psoriasis, especially in severe cases, can increase the risk of cardiovascular problems.
- Concerns: This includes heart disease, high blood pressure, and stroke.
- Reason: Chronic inflammation associated with psoriasis may contribute to artery damage.
Eye Conditions
Psoriasis can increase the risk of certain eye disorders.
- Disorders: These include conjunctivitis, blepharitis, and uveitis.
Mental Health Effects
The impact of psoriasis on appearance and life quality can lead to psychological effects.
- Effects: Depression, anxiety, and feelings of low self-esteem are common. People with psoriasis are nearly twice as likely to experience depression as those without the disease
Other Autoimmune Diseases
People with psoriasis are more likely to develop other immune-mediated conditions.
- Diseases: These can include celiac disease, sclerosis, and the inflammatory bowel disease Crohn’s.
Metabolic Syndrome
A cluster of conditions that increase the risk of heart disease, stroke, and type 2 diabetes.
- Components: High blood pressure, obesity, elevated insulin levels, and abnormal cholesterol levels.
Psoriasis, though often classified as a skin disorder, carries the potential for numerous complications, emphasizing the importance of effective management and treatment.
Life with Psoriasis
Individuals with psoriasis often face challenges that span both physical and emotional realms. The disease’s manifestations can influence various aspects of a person’s life, from daily routines to social interactions.
Physical Adjustments
Daily Activities: Psoriasis can make routine activities, such as dressing or showering, uncomfortable or painful, especially during flare-ups.
Physical Discomfort: Symptoms like itching, burning, or bleeding can cause persistent discomfort, requiring constant management.
Emotional Well-being
Self-esteem and Body Image: Visible psoriasis patches can affect an individual’s confidence and how they perceive themselves.
Mental Health: There’s an increased risk of anxiety and depression among individuals with psoriasis, largely due to the condition’s chronic nature and its visible manifestations.
Social Implications
Interpersonal Relationships: Due to the appearance of their skin or concerns about how others might react, some people with psoriasis might avoid social situations or intimate interactions.
Public Perception: Misunderstandings about the disease can lead to unwarranted stigmatization. Educating others becomes a regular task for many with psoriasis.
Work and Productivity
Career Impact: Flare-ups or medical appointments related to psoriasis might require time off work, potentially influencing job performance and opportunities.
Workplace Interactions: Visible symptoms might prompt questions or concerns from colleagues, requiring explanations or setting boundaries.
Management and Treatment
Routine: Regular treatments, whether topical, oral, or biologic, become integral to a person’s routine.
Financial Considerations: Persistent treatments can lead to significant medical expenses, especially if insurance doesn’t cover specific medications or therapies.
Living with psoriasis requires strength, understanding, and adaptability. By fostering supportive environments and spreading awareness, society can make the journey easier for those affected. An informed community, combined with advanced medical interventions, ensures a brighter future for individuals with psoriasis.
Final Thoughts
Psoriasis, a chronic skin condition, significantly affects many individuals worldwide. While its physical symptoms can be evident, its emotional and psychological implications can be equally challenging.
Continuous research and medical advancements provide hope for improved treatments and understanding. As awareness grows, those with psoriasis can look forward to society more informed about their condition, leading to better support and reduced stigma.
It’s essential for affected individuals to remain proactive in their care and for the broader community to be empathetic and understanding.
FAQs
Sources
- NIAMS. “Psoriasis.” National Institute of Arthritis and Musculoskeletal and Skin Diseases, 12 Apr. 2017, www.niams.nih.gov/health-topics/psoriasis Accessed 1 Oct. 2023. ↩︎
- “Psoriasis: Signs and Symptoms.” Www.aad.org, 1 Oct. 2023, www.aad.org/public/diseases/psoriasis/what/symptoms Accessed 1 Oct. 2023.
↩︎ - McNulty, Maureen, et al. “T Cells in Psoriasis: A Simplified Guide.” Mypsoriasisteam.com, MyPsoriasisTeam, 27 May 2022, www.mypsoriasisteam.com/resources/t-cells-in-psoriasis-a-simplified-guide. Accessed 1 Oct. 2023. ↩︎
- “Psoriasis: Causes.” Www.aad.org, 1 Oct. 2023, www.aad.org/public/diseases/psoriasis/what/causes. Accessed 1 Oct. 2023. ↩︎
- Mayo Clinic. “Psoriasis – Symptoms and Causes.” Mayo Clinic, 2022, www.mayoclinic.org/diseases-conditions/psoriasis/symptoms-causes/syc-20355840#:~:text=Psoriasis%20is%20a%20skin%20disease Accessed 1 Oct. 2023.
↩︎ - “National Psoriasis Foundation – Home.” Www.psoriasis.org, 1 Oct. 2023, www.psoriasis.org/. Accessed 1 Oct. 2023. ↩︎
- WebMD. “Psoriasis.” WebMD, WebMD, 3 Dec. 2001, www.webmd.com/skin-problems-and-treatments/psoriasis/understanding-psoriasis-basics Accessed 1 Oct. 2023.
↩︎ - Cleveland Clinic. “Psoriasis | Cleveland Clinic.” Cleveland Clinic, 2016, my.clevelandclinic.org/health/diseases/6866-psoriasis. Accessed 1 Oct. 2023.
↩︎