The human brain, with its intricate web of neurons, serves as the control center for all functions of the body. To keep it operating efficiently, it requires a continuous supply of oxygen and nutrients, which are delivered through the bloodstream. But what happens when this blood supply gets interrupted? The answer is a stroke.
What is Stroke?
A stroke is a medical emergency where the blood supply to a part of the brain is reduced or interrupted, leading to brain cell damage. It can result from a blocked artery (ischemic stroke) or the leaking or bursting of a blood vessel (hemorrhagic stroke). It is the fifth leading cause of death and the top cause of disability in the United States1.
Stroke carries a high risk of death. Survivors may face vision loss, speech difficulties, paralysis, and cognitive issues. There’s an increased risk of subsequent strokes for those with one. The type of stroke determines its severity:
- Transient Ischaemic Attacks (TIA) resolve within a day.
- Carotid Stenosis Stroke is due to a narrowed neck artery.
- Ischemic Stroke results from artery blockage.
- Hemorrhagic Stroke, caused by a ruptured brain vessel, is the most lethal.
Each year, 15 million people globally experience a stroke. 5 million die and 5 million sustain long-term disabilities. Strokes are uncommon for those under 40 but are primarily caused by hypertension when they do occur. Additionally, 8% of children with sickle cell disease suffer from strokes.
The leading preventable risk factors are high blood pressure and smoking. Proper blood pressure control could prevent many stroke-related deaths.
For those under 65, smoking is linked to 40% of stroke fatalities. Despite a decrease in stroke rates in developed countries, the total number of cases is rising due to an aging population.2
Different Types and Causes
Here are the different types of strokes and their respective causes:3
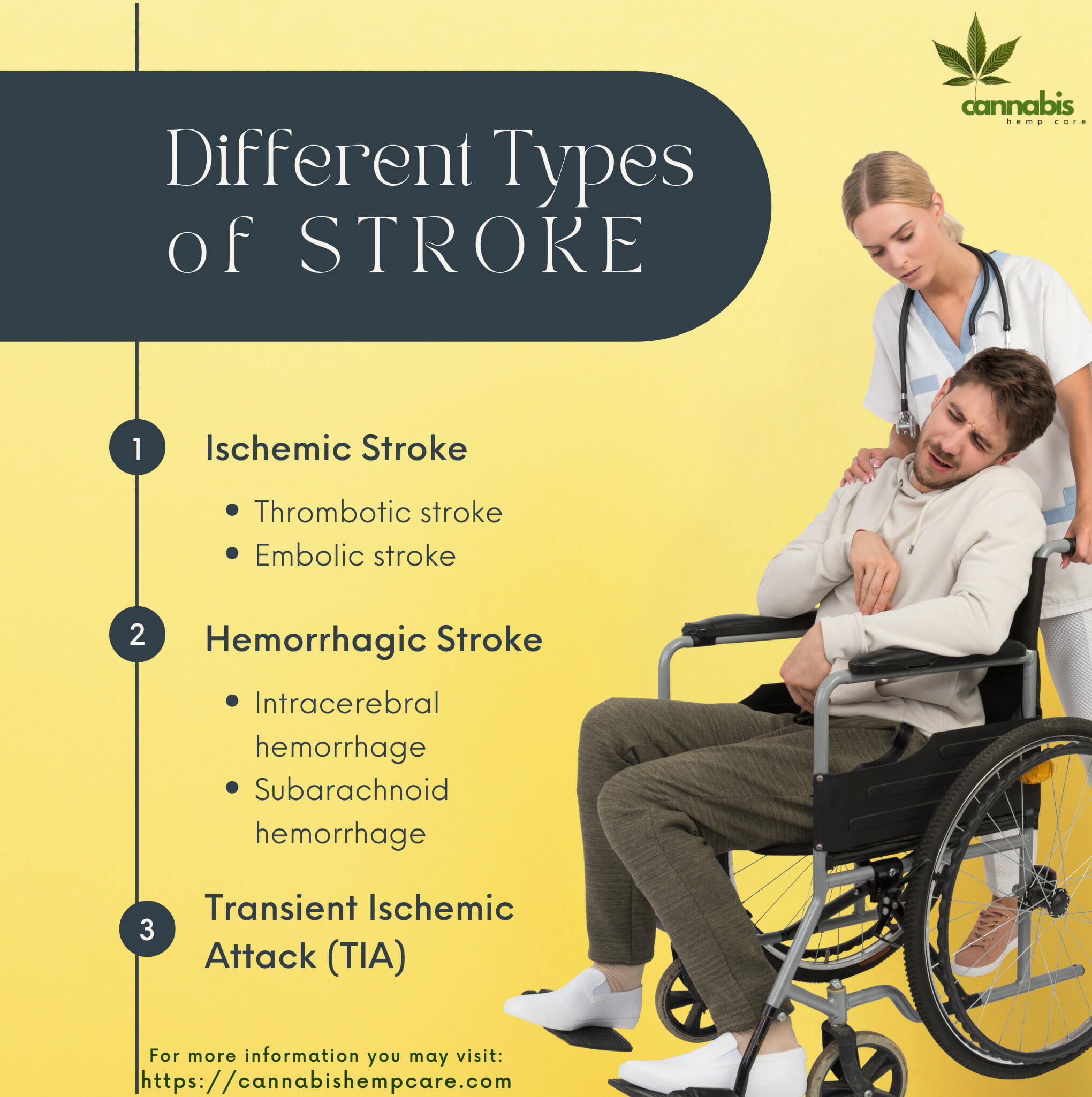
- Ischemic Stroke: Represents about 85% of strokes. It’s caused by blockages (often blood clots) that reduce blood flow to the brain. These blockages can arise from two sources:
- Thrombotic stroke: Caused by a clot forming in an artery directly supplying the brain.
- Embolic stroke: Caused by a clot or debris originating elsewhere, usually the heart, which then migrates to brain arteries.
- Thrombotic stroke: Caused by a clot forming in an artery directly supplying the brain.
- Hemorrhagic Stroke: Caused by bleeding in the brain due to a burst blood vessel. It can be further categorized as:
- Intracerebral hemorrhage: Bleeding directly within the brain.
- Subarachnoid hemorrhage: Bleeding between the brain and the surrounding protective tissue.
- Intracerebral hemorrhage: Bleeding directly within the brain.
- Transient Ischemic Attack (TIA): Often dubbed a “mini-stroke,” it results from temporary blockages. While not causing permanent damage, it’s a warning sign and a precursor to potential full-blown strokes.
Symptoms and Warning Signs
Recognizing stroke symptoms promptly can mean the difference between full recovery and long-term disability. Strokes are a medical emergency, and the faster you identify and act on the symptoms, the better the chances of minimizing brain damage and potential complications.
1. The Basics of “FAST”
- Face: A sudden numbness or weakness on one side of the face, often manifesting as a drooping mouth or eye, is a red flag. This facial asymmetry can be a clear indication of a stroke.
- Arms: Numbness or weakness in one arm or an inability to raise it fully can be another warning sign. This might also extend to the leg on the same side.
- Speech: Difficulty in speaking or understanding speech is a common stroke symptom. Slurred speech or an inability to correctly repeat a simple sentence can indicate a problem with brain function.
- Time: Every minute counts when it comes to stroke treatment. Immediate medical intervention increases the chances of a full recovery and reduces the extent of potential damage.
2. Warning Signs Of A Stroke
While “FAST” covers the most common and easily recognizable symptoms, there are other signs that you should be aware of:
- Sudden Confusion: Abrupt difficulty understanding speech or unexplained confusion about time or place.
- Trouble Seeing: Sudden blurred or blackened vision in one or both eyes or double vision.
- Walking Difficulties: A sudden loss of balance, dizziness, or trouble walking.
- Severe Headache: A sudden, severe headache, often described as the “worst headache of my life,” can indicate a hemorrhagic stroke or brain aneurysm rupture.
- Nausea or Vomiting: While less common, sudden nausea or vomiting, especially when combined with other symptoms, can indicate a stroke.
- Numbness: A sudden numbness or lack of sensation in parts of the body, especially on one side.
Recognizing stroke symptoms and acting swiftly is crucial4. The sooner the intervention, the better the outcome. Whether you’re relying on the “FAST” method or noticing other concerning symptoms, always prioritize seeking medical attention. Remember, it’s better to be safe than sorry.

Foods That Trigger Stroke
Certain foods can trigger an increased risk of stroke due to their composition and the impact they have on one’s cardiovascular health. Here is a list of food triggers that are known to be associated with a higher stroke risk, along with explanations of how they contribute to this serious health concern:
1. Sodium (Salt):
Excessive sodium, predominantly from processed foods, canned products, and many restaurant offerings, is a notable contributor to high blood pressure, a primary risk factor for stroke.
2. Trans and Saturated Fats:
These fats, frequently found in processed snacks, certain baked goods, fast-food selections, and some spreads, can elevate LDL cholesterol. This potentially leads to atherosclerosis, characterized by arterial narrowing and hardening, increasing the risk of stroke.
3. Processed Meats:
Foods like bacon, sausages, and certain deli choices are sodium-rich and contain preservatives. These attributes might contribute to higher blood pressure and cholesterol levels.
4. Red Meat:
Regular intake, especially of fatty or heavily processed varieties, has connections with atherosclerosis.
5. Fried Foods:
Popular items like fried chicken, fries, and doughnuts often contain fats that aren’t heart-healthy and can introduce more dietary cholesterol.
6. Sugary Beverages:
Overconsumption of drinks like sodas, overly sweet teas, and certain fruit drinks may result in weight issues, potential diabetes onset, and increased blood pressure.
7. Alcohol Intake:
While moderation might offer cardiovascular benefits, excessive drinking can exacerbate blood pressure levels, heightening stroke risk.
8. Refined Carbohydrates and Sugars:
Staples such as white bread, white rice, and high-sugar cereals might cause abrupt blood sugar surges, which over time are associated with heart and arterial complications.
9. Commercial Baked Goods:
These often contain unhealthy fats and sugars, impacting cholesterol levels and overall arterial health.
10. Certain Sweeteners:
There’s ongoing research, but some findings indicate that excessive consumption of particular artificial sweeteners may be linked to heightened stroke risk.
Balancing out these risk-increasing foods by emphasizing a diet abundant in fruits, vegetables, whole grains, and lean proteins can be a preventive measure. The Mediterranean Diet and the DASH Diet are both reputable for promoting heart and brain wellness.
Risk factors
Understanding the risk factors for a stroke is crucial for prevention and early intervention. These risk factors can be broadly categorized into two groups: modifiable and non-modifiable.
Non-Modifiable Risk Factors
- Age: The risk of stroke doubles for each decade after the age of 55. Although it’s more common in older adults, people of all ages, including children, can experience a stroke.
- Heredity and Race: If your parent, grandparent, sister, or brother has had a stroke – especially before reaching age 65 – you may be at greater familial risk. Certain races also have a higher risk. For instance, African Americans have a much higher risk of death from a stroke than Caucasians, partly because of a higher prevalence of hypertension and diabetes.
- Gender: Historically, more women than men have strokes yearly, partly because women live longer.
- Prior Stroke or TIA: Individuals who’ve previously experienced a stroke or a transient ischemic attack (TIA) have a much higher risk of having another.
Modifiable Risk Factors
- Hypertension: This is the most potent risk factor for stroke. Managing blood pressure is crucial for preventing both ischemic and hemorrhagic strokes.
- Tobacco Use: Smoking or passive exposure to smoke can damage blood vessels, leading to blockages that can cause a stroke. The nicotine and carbon monoxide in tobacco also decrease the amount of oxygen reaching the brain.
- Diabetes: Diabetes increases the risk of stroke, mainly because it’s associated with other conditions like obesity, high blood pressure, and high cholesterol.
- Cardiovascular Diseases: Conditions like coronary artery disease, heart valve disease, atrial fibrillation, and certain types of cardiomyopathies can increase the risk of clot formation and subsequent ischemic stroke.
- High Cholesterol: Elevated cholesterol levels can contribute to artery-clogging plaques that can cause a stroke.
- Physical Inactivity and Obesity: Being inactive, obese, or both can elevate your risk of high blood pressure, high blood cholesterol, diabetes, heart disease, and stroke.
- Excessive Alcohol or Illegal Drug Use: Consuming more than 2 drinks per day can lead to high blood pressure. Drugs like cocaine and methamphetamines are also known to elevate stroke risks.
- Obstructive Sleep Apnea (OSA): OSA, a condition where breathing repeatedly stops and starts during sleep, can contribute to various complications, including stroke.
- Other Factors: Chronic kidney disease, inflammatory conditions, high levels of homocysteine (an amino acid in the blood), and certain blood disorders can also be contributory.

Treatment Approaches
The right treatment for a stroke depends on its type: ischemic, hemorrhagic, or transient ischemic attack (TIA). Early identification and immediate medical intervention can make a significant difference in patient outcomes.
1. Ischemic Stroke
Ischemic strokes account for nearly 85% of all strokes. They occur when a blood vessel supplying the brain becomes blocked, typically by a clot.
Medications:
- Clot-busting drugs (Thrombolytics): The most commonly used drug for thrombolytic therapy is tissue plasminogen activator (tPA), or alteplase. Administered through an IV in the arm, it works by dissolving the clot and restoring blood flow to the affected region. To be most effective, this drug must be given within 4.5 hours after stroke symptoms begin.
Procedures:
- Endovascular procedures: These are minimally invasive procedures performed within the blood vessels. A catheter is threaded through an artery in the groin up to the blocked artery in the brain. The clot can then be removed or dissolved, depending on the circumstances.
- Carotid endarterectomy: For patients with narrowing or blockage of the carotid arteries (major arteries in the neck that supply blood to the brain), this surgery involves the removal of atherosclerotic plaques.
2. Hemorrhagic Stroke
Hemorrhagic strokes result from bleeding within the brain or between the brain and the skull. Their treatment focuses on controlling the bleeding, reducing the pressure in the brain, and stabilizing vital signs, especially blood pressure.
Medications:
- Drugs to lower brain pressure: To reduce swelling, medications like mannitol or hypertonic saline can be administered.
- Drugs to reduce blood pressure: Tight blood pressure control is crucial, and medications such as beta-blockers, ACE inhibitors, or diuretics can be employed.
- Anti-seizure drugs: Hemorrhagic strokes can increase the risk of seizures. Antiepileptic drugs like phenytoin or levetiracetam might be used to address this.
Surgery:
- Surgical clipping: Used to prevent blood flow to an aneurysm, a metal clip is placed at the base of the aneurysm.
- Endovascular coiling (embolization): This procedure involves inserting a catheter into an artery in the groin, guiding it to the brain using X-ray imaging, and depositing a tiny coil into the aneurysm, promoting blood clotting and reducing the risk of rupture.
- Stereotactic radiosurgery: An option for some brain aneurysms and arteriovenous malformations, it employs multiple beams of highly focused radiation to repair vascular malformations.
- Hematoma removal: In cases where a large blood collection builds up within the brain, surgery might be required to remove it and reduce pressure.
3. Transient Ischemic Attack (TIA)
While TIAs do not cause permanent damage, they are a warning sign of a future stroke and shouldn’t be ignored.
- Anti-platelet drugs: These are the most commonly prescribed medications for TIA patients, reducing the risk of a future ischemic stroke by making platelets less sticky and less likely to clot. Examples include aspirin, clopidogrel (Plavix), and aspirin combined with extended-release dipyridamole.
- Anticoagulants: In certain cases, like when atrial fibrillation is identified, drugs like warfarin or newer anticoagulant medications might be prescribed.
- Other treatments: Depending on the cause of the TIA, other treatments may be required. This can range from carotid endarterectomy or angioplasty (for a blocked neck artery) to medications to control contributing factors such as hypertension or diabetes.
The treatment landscape for stroke is evolving rapidly, with advancements in medical technology and pharmacology offering hope to those affected. The key to maximizing these treatments lies in early detection and timely medical intervention. Remember, in the context of a stroke, every second saved is brain function preserved.
Foods That Lower Stroke Risk
Diet plays a significant role in influencing stroke risk. Here are foods that have been identified to lower the risk of stroke potentially and the reasons behind their beneficial effects:
1. Leafy Greens:
Spinach, kale, and chard are rich in antioxidants, fiber, and vital minerals, helping to support healthy blood pressure and vascular function.
2. Whole Grains:
Oats, barley, and quinoa, among others, can help regulate blood sugar levels and maintain a healthy weight, both crucial for reducing stroke risk.
3. Fatty Fish:
Salmon, mackerel, and sardines are packed with omega-3 fatty acids, which have been linked to decreased inflammation and improved heart health.
4. Berries:
Blueberries, strawberries, and raspberries contain compounds that may reduce blood pressure and prevent clotting.
5. Nuts and Seeds:
Almonds, walnuts, and flaxseeds are great sources of beneficial fats, fibers, and antioxidants that support heart and brain health.
6. Legumes:
Beans, lentils, and chickpeas are high in fiber and protein, supporting healthy blood pressure and cholesterol levels.
7. Olive Oil:
A cornerstone of the Mediterranean diet, olive oil is linked to reduced inflammation and better heart health.
8. Avocado:
Rich in heart-healthy monounsaturated fats and potassium, avocados can assist in managing blood pressure.
9. Dark Chocolate:
Cocoa, particularly in higher-concentration dark chocolate, contains flavonoids that may boost heart health, but moderation is key.
10. Citrus Fruits:
Oranges, grapefruits, and lemons are high in vitamin C and flavonoids, potentially reducing stroke risk.
11. Tea:
Both green and black teas have compounds that could lower risks associated with high blood pressure and cholesterol.
While these dietary choices can be beneficial, it’s essential to consider the whole diet and lifestyle. Regular exercise, maintaining a healthy weight, and avoiding smoking and excessive alcohol are also crucial. As always, consult with healthcare professionals when considering dietary changes and to understand individual risk factors.

Rehabilitation and Life Post-Stroke
Recovering from a stroke is an individualized journey, varying from one person to another based on the stroke’s severity, affected brain region, and the individual’s overall health. Rehabilitation is a crucial phase of this recovery process, aiming to help stroke survivors regain lost skills and learn to cope with the challenges that may arise.
1. Rehabilitation Goals
The primary objectives of stroke rehabilitation include:
- Regaining lost motor skills: Improving muscle strength, coordination, and the patient’s ability to move effortlessly.
- Enhancing speech and cognitive functions: Speech therapists work to restore language skills, while cognitive therapy aims to improve impaired abilities like memory, attention, and problem-solving.
- Achieving functional independence: The ultimate goal is to help patients become as independent as possible, enhancing their quality of life.
- Emotional and psychological well-being: Addressing emotional challenges, such as depression, anxiety, or feelings of grief and frustration, is equally essential in the rehabilitation process.
2. Rehabilitation Therapies
- Physical Therapy: Helps patients regain previously learned motor skills and improve muscle strength and coordination5.
- Occupational Therapy: Focuses on improving daily activities such as dressing, eating, bathing, and writing.
- Speech Therapy: Assists in regaining lost language and speech skills. It can also help with swallowing difficulties, a common post-stroke issue.
- Neuropsychology and Cognitive Therapy: Addresses problems with memory, attention, problem-solving, and judgment.
- Recreational Therapy: Encourages participation in leisure activities and offers an avenue for social interaction.
- Vocational Therapy: Helps individuals return to their former jobs or find new employment that suits their post-stroke capabilities.
3. Adapting to Life Post-Stroke
Life after a stroke can mean adjusting to physical, cognitive, or emotional changes. These adaptations may include:
- Home modifications: Making homes more accessible with ramps, handrails, and specialized bathroom equipment.
- Use of assistive devices: Wheelchairs, braces, walking aids, and communication aids can help survivors in their daily tasks.
- Lifestyle changes: Adopting a healthier lifestyle by maintaining an appropriate diet, engaging in physical activity, abstaining from smoking, and moderating alcohol consumption.
- Joining support groups: Connecting with other stroke survivors can offer emotional support and provide a platform to share experiences and coping techniques.
- Routine medical check-ups: Regular screenings and medications help in preventing another stroke and managing other potential health issues.
4. Emotional and Psychological Recovery
- Psychotherapy: Speaking with a therapist can help address feelings of depression, anxiety, and anger that are common post-stroke.
- Medication: Some stroke survivors may benefit from antidepressants or anxiety-reducing medicines.
- Mindfulness and relaxation techniques: Meditation, deep breathing exercises, and other relaxation techniques can help manage emotional challenges.
Recovery and rehabilitation post-stroke can be a long and challenging process. It’s a journey of resilience, adaptability, and hope. With the right support system, medical intervention, and therapies, many stroke survivors can regain their independence and lead fulfilling lives.
Building awareness about the importance of rehabilitation can foster a supportive community that stands alongside stroke survivors, cheering them on every step of the way.
Prevention
Preventing a stroke is always better than treating one. This involves:
1. Risk Factor Management
- Hypertension Control: High blood pressure is a leading cause of stroke. Regular monitoring and medications like ACE inhibitors, beta-blockers, and diuretics can manage it.
- Blood Sugar Levels: Diabetes increases stroke risk. Medications, lifestyle changes, and regular monitoring can keep it in check.
- Cholesterol Management: High cholesterol can lead to artery-clogging plaques. Statins and other medications can help reduce cholesterol levels.
2. Lifestyle Interventions
- Diet: A balanced diet rich in fruits, vegetables, and whole grains, and low in saturated fats, helps prevent stroke.
- Physical Activity: Regular exercise, even moderate in intensity, reduces stroke risk.
- Limit Alcohol and Quit Smoking: Both are significant stroke risk factors. Reducing alcohol consumption and quitting smoking can significantly reduce the risk.
3. Medications and Therapies
- Antiplatelet agents: Drugs like aspirin or clopidogrel help reduce the risk of blood clots, especially in those who’ve had a TIA or minor ischemic strokes.
- Anticoagulants: Medications like warfarin, dabigatran, or apixaban prevent clot formation, especially crucial for those with atrial fibrillation6.
4. Monitoring and Detection
- Atrial Fibrillation Monitoring: Irregular heartbeats can cause clots. Wearable technology and implantable devices now allow for more extended and precise monitoring.
- Carotid Ultrasound: This non-invasive test detects blockages or narrowing in the carotid arteries and can identify individuals at higher risk.
5. Surgical Interventions
- Carotid Endarterectomy: A procedure to remove plaque from the carotid arteries, preventing strokes in high-risk individuals.
- Angioplasty and Stents: Widening narrowed arteries and placing a mesh to prevent them from narrowing again.
6. Emerging Technologies
- Telemedicine: Enables early stroke diagnosis, especially in remote areas, ensuring timely treatment.
- AI and Machine Learning: Innovative software helps in quicker analysis of brain scans, leading to faster diagnosis and treatment decisions.
Prevention is the cornerstone of the fight against stroke. Prevention is better than cure.

Final Thoughts
Stroke is not just a medical condition; it’s a stark reminder of the fragile balance within our bodies. The brain, our most vital organ, is both resilient and vulnerable. As we continue to learn more about stroke, its causes, and its aftermath, it’s paramount to prioritize early detection and preventive measures.
By understanding stroke, we empower ourselves to make informed decisions that safeguard our health and well-being. Knowledge, after all, is our strongest defense against the unexpected turns of life.
FAQs
Sources
- American Stroke Association. “About Stroke.” American Stroke Association, 2022, www.stroke.org/en/about-stroke. Accessed 1 Oct. 2023. ↩︎
- World Health Organization. “WHO EMRO | Stroke, Cerebrovascular Accident | Health Topics.” World Health Organization – Regional Office for the Eastern Mediterranean, 2022, www.emro.who.int/health-topics/stroke-cerebrovascular-accident/index.html. Accessed 1 Oct. 2023 ↩︎
- Centers For Disease Control and Prevention. “Learn about Stroke.” Centers for Disease Control and Prevention, 2 Aug. 2021, www.cdc.gov/stroke/about.htm#:~:text=A%20stroke%2C%20sometimes%20called%20a. Accessed 1 Oct. 2023. ↩︎
- Cleveland Clinic. “Stroke: What It Is, Causes, Symptoms, Treatment & Types.” Cleveland Clinic, 22 Sept. 2022, my.clevelandclinic.org/health/diseases/5601-stroke. Accessed 1 Oct. 2023. ↩︎
- “Stroke: Causes, Symptoms, Diagnosis, and Treatment.” Www.medicalnewstoday.com, 1 Oct. 2023, www.medicalnewstoday.com/articles/7624#treatment. Accessed 1 Oct. 2023. ↩︎
- Robert Brown. “Stroke – Symptoms and Causes.” Mayo Clinic, 20 Jan. 2020, www.mayoclinic.org/diseases-conditions/stroke/symptoms-causes/syc-20350113. Accessed 1 Oct. 2023. ↩︎