Rheumatoid Arthritis (RA) is like an uninvited guest that suddenly shows up at a party. Just when you think you’re having a good day, RA symptoms can flare up, causing pain and discomfort. But what causes these sudden bursts? Let’s delve into the common triggers and how to navigate them.
So, What Exactly Is Rheumatoid Arthritis?
RA is an autoimmune disorder, which means your immune system, instead of defending against external threats, mistakenly attacks your own joints. This leads to inflammation, causing pain, swelling, and eventually joint damage. Imagine your body’s defense system getting its wires crossed and seeing your joints as the enemy.
What Are the Main Triggers for RA Symptoms?
Let’s delve deeper into each of the triggers for Rheumatoid Arthritis (RA) symptoms, providing a more comprehensive understanding of the factors that can exacerbate RA:
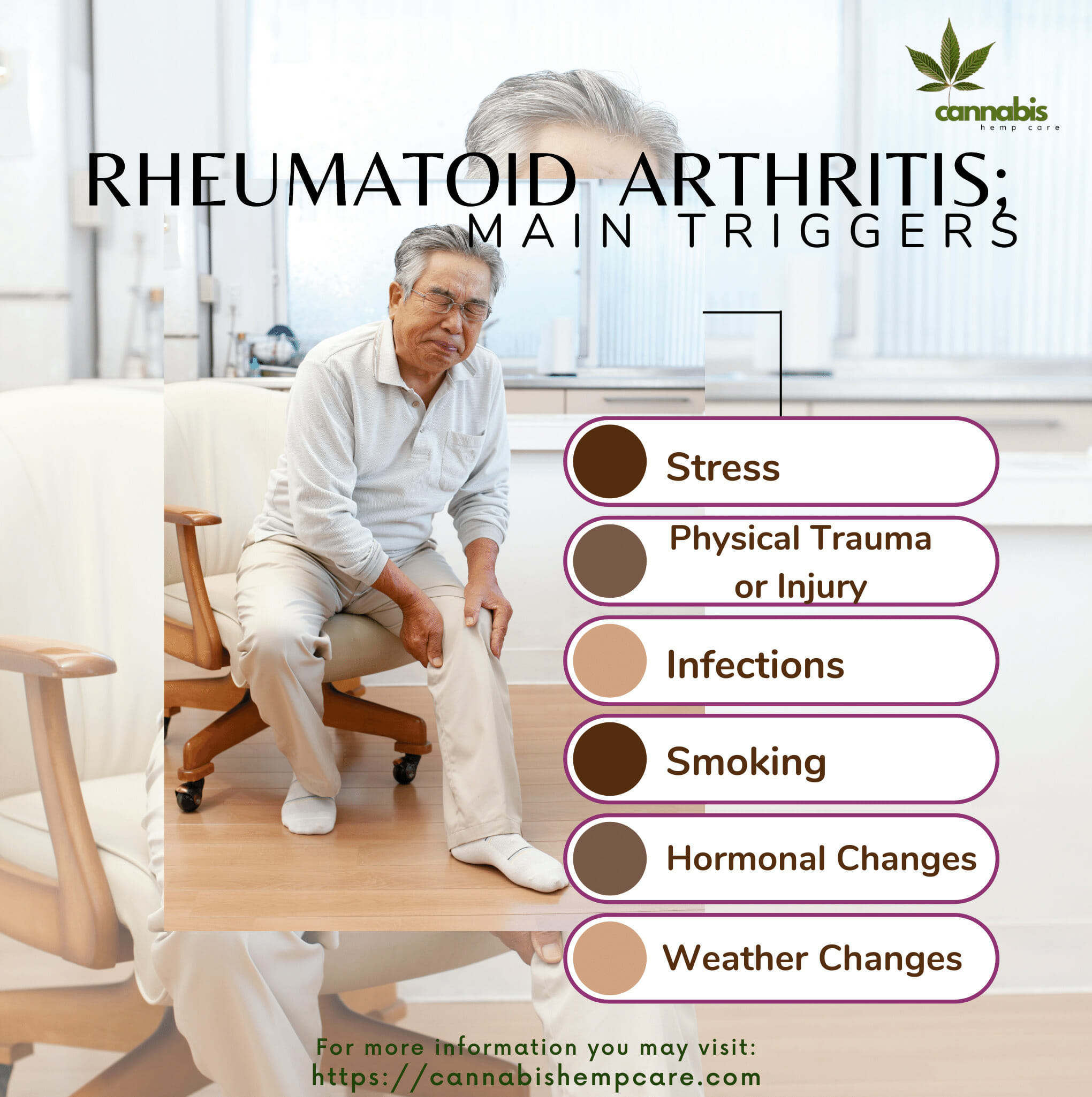
- Stress: Chronic stress leads to the production of stress hormones like cortisol. When the body is constantly in a state of stress, the immune system can become dysregulated, and in people with RA, this can lead to increased inflammation in the joints. Furthermore, according to a study in the journal Brain, Behavior, and Immunity, chronic stress can alter the function of immune cells, making them more prone to promote inflammation.
- Physical Trauma or Injury: When there’s a physical injury, the body’s immune response gets activated to repair the damage. In the case of RA, this immune response can become overactive and mistakenly target the joints, causing inflammation. This explains why a sprain or joint injury can trigger an RA flare-up. The inflammation that accompanies the injury may intensify the ongoing inflammation in people with RA.
- Infections: When you have an infection, your immune system goes into high gear to fight it off. But in people with RA, the immune system is already misdirected towards attacking the joints. So when an infection occurs, it can exacerbate the immune response, leading to increased inflammation in the joints. The journal Clinical Rheumatology has published research indicating that certain infections, such as Epstein-Barr virus and periodontal bacteria, may trigger the onset of RA in genetically predisposed individuals.
- Smoking: Cigarette smoke contains numerous harmful substances that can increase inflammation in the body. In people with RA, smoking can make symptoms worse and increase the severity of the disease. A study in the journal Rheumatology found that smokers with RA had higher levels of certain inflammatory markers and more severe joint damage compared to non-smokers with RA. Moreover, smoking can also reduce the effectiveness of some RA medications.
- Hormonal Changes: Hormones like estrogen have immunomodulatory effects, meaning they can influence the activity of the immune system. Fluctuations in hormone levels during the menstrual cycle or menopause can affect the immune response in women with RA. Some women may experience increased joint pain and inflammation during periods of hormonal change. Research in the journal Autoimmunity Reviews has explored the complex relationship between hormones and autoimmune diseases like RA.
- Weather Changes: Some people with RA report that their symptoms get worse when the weather changes, especially during cold or damp conditions. While the exact mechanism is unclear, it’s believed that changes in atmospheric pressure might affect the fluid balance in the joints, leading to increased pain and stiffness. However, the relationship between weather and RA symptoms is still a topic of ongoing research, and studies have produced mixed results.
Understanding these triggers and how they affect RA symptoms is crucial for managing the disease. Working with a healthcare professional to identify and address personal triggers can help individuals with RA reduce the frequency and intensity of flare-ups.

How Can I Avoid These Triggers?
While it’s impossible to avoid every potential trigger, being aware and proactive can help:
- Stay Calm and Relaxed: Engage in relaxation techniques like meditation or deep-breathing exercises. Reducing stress can help manage RA symptoms.
- Watch Your Physical Activities: It’s important to be active, but overexertion can lead to injuries. Consult a physical therapist to find a regimen suitable for you.
- Maintain Good Hygiene: Simple practices, like regular hand-washing, can prevent infections.
- Quit Smoking: If you’re a smoker, seek help to quit. Your joints (and lungs) will thank you!
- Track Your Symptoms: Maintain a diary. By noting when and under what circumstances your symptoms worsen, you can identify personal triggers.

Are There Dietary Triggers?
Yes! Certain foods can worsen RA symptoms:
Diet and Food Sensitivities:
Certain foods can aggravate RA symptoms in some people. For example:
- Processed Foods and Sugars: These can increase inflammation in the body. According to the Arthritis Foundation, consuming sugar and processed foods may trigger the release of inflammatory cytokines.
- Dairy Products: Some people with RA have found that eliminating dairy or opting for dairy substitutes can help reduce their symptoms. It’s believed that certain proteins in dairy might irritate the tissue around the joints.
- Red Meat and Fried Foods: Foods high in saturated fats, like red meat and fried foods, can increase inflammation. A study in the Journal of the American Dietetic Association suggested that reducing the intake of fried and processed foods can help reduce inflammation and thus help with RA symptoms.

Medication Side Effects:
Some medications, even those intended for other health conditions, can exacerbate RA symptoms. It’s always important to:
- Monitor New Medications: Whenever you’re prescribed a new medication, observe any changes in your RA symptoms.
- Discuss with Your Rheumatologist: Your doctor can provide insights into potential interactions or side effects that can affect your RA.
Sleep and Fatigue:
A good night’s sleep is essential for everyone, but especially for those with RA.
- Sleep Quality: According to a study in the Journal of Clinical Sleep Medicine, poor sleep can heighten pain sensitivity and exacerbate joint pain.
- Rest and Recovery: Make sure to get adequate rest, especially after physically demanding days, to help your body recover and to prevent potential flare-ups.
Emotional Factors:
- Mental Health: Conditions like anxiety and depression can indirectly impact RA. The Arthritis Foundation notes that depression is more common among people with RA compared to the general population. This emotional burden can, in turn, exacerbate physical symptoms.
- Support Systems: Having a strong support system, whether through family, friends, or RA support groups, can help in managing both the emotional and physical challenges of the disease.
By recognizing and addressing these additional triggers, individuals with RA can have a more comprehensive approach to managing their symptoms. It’s essential to work closely with a healthcare provider and consider personal lifestyle factors that might be contributing to RA flare-ups.

In Conclusion
Understanding your RA triggers is like having a roadmap. It won’t prevent every flare-up, but it’ll give you the tools to navigate them better. Remember, everyone’s experience with RA is unique. With awareness, a positive attitude, and a proactive approach, you can lead a fulfilling life despite RA. Stay informed and stay proactive!
FAQs
What are the best vitamins for rheumatoid arthritis?
Vitamin D: Supports bone health.
Omega-3 Fatty Acids: Reduces inflammation.
Vitamin E: May decrease inflammation.
Vitamin C: Boosts the immune system and aids joint health.
How to boost the immune system with rheumatoid arthritis?
Maintain a balanced diet.
Engage in low-impact exercises.
Prioritize sleep.
Manage stress.
Stay hydrated.
Are eggs beneficial for rheumatoid arthritis?
Eggs provide protein but can promote inflammation in excess. Monitor your body’s response.
What worsens rheumatism?
Factors include stress, trauma, infections, smoking, certain foods, lack of sleep, and some medications.
Can rheumatoid arthritis patients eat chicken?
Yes, but choose lean preparations like baked or grilled. Monitor for any symptom triggers.